ST段抬高一定是心肌梗死吗?
2018-02-15 熊长明 肺血管病
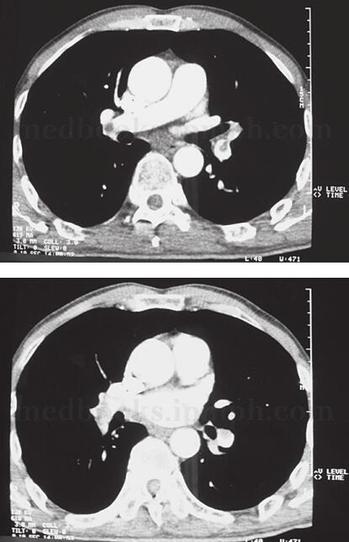
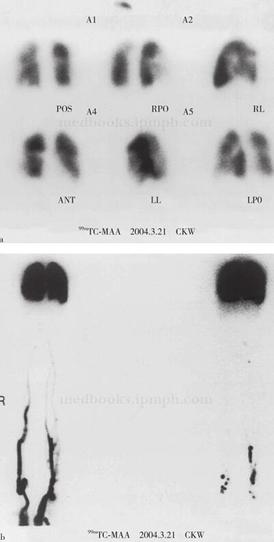
尽管急性肺血栓栓塞症(急性肺栓塞)心电图(ECG)改变是非特异性的,但在急性肺栓塞的诊断和鉴别诊断中仍具有重要价值。不少急性肺栓塞的ECG表现为胸前导联的T波倒置,但表现为ST段抬高者非常少见。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言




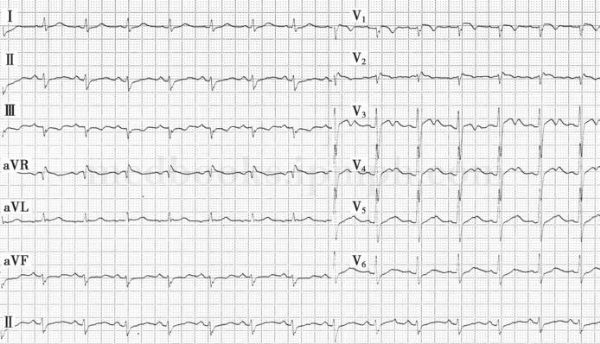
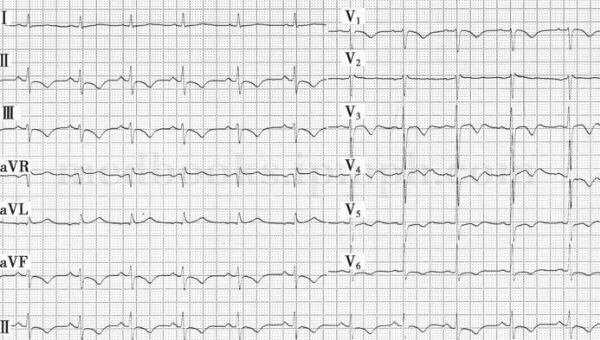





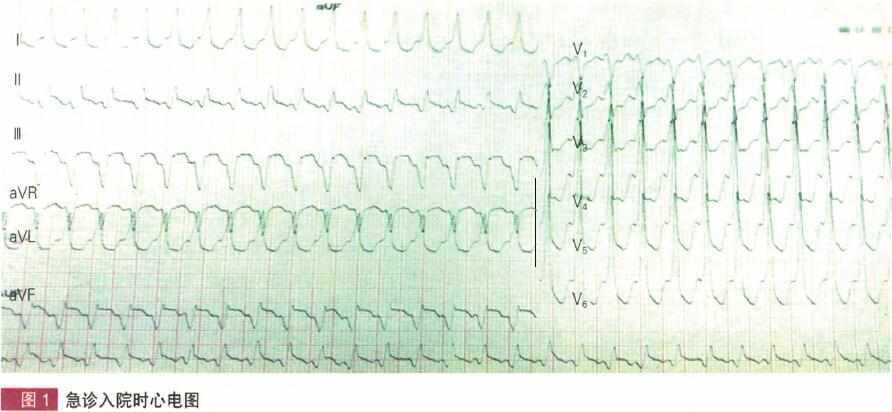




ST段抬高心电图解析.
72
#ST段抬高#
51
#ST段#
37
好文章.学习了.
63
学习了.获益匪浅!感谢分享
66