Heart:主动脉缩窄成年幸存者的长期死亡率和心血管负担
2019-03-29 xiangting MedSci原创
缩窄修复当代成人幸存者的长期生存率显著低于匹配的正常人群,并在第三个10年后加速下降。
这项研究旨在探讨缩窄修复术后的当代长期预后。
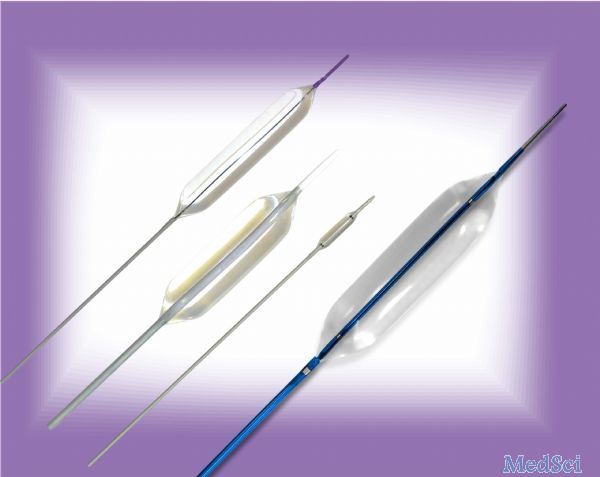
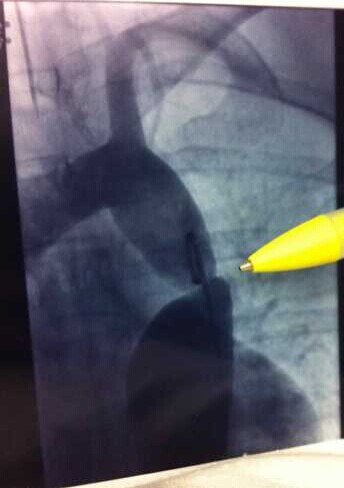
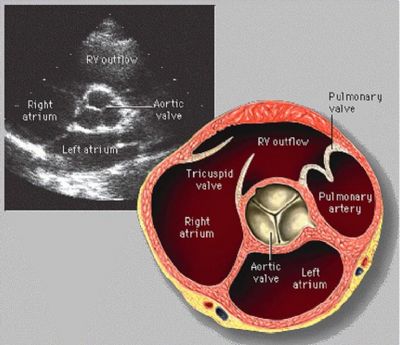
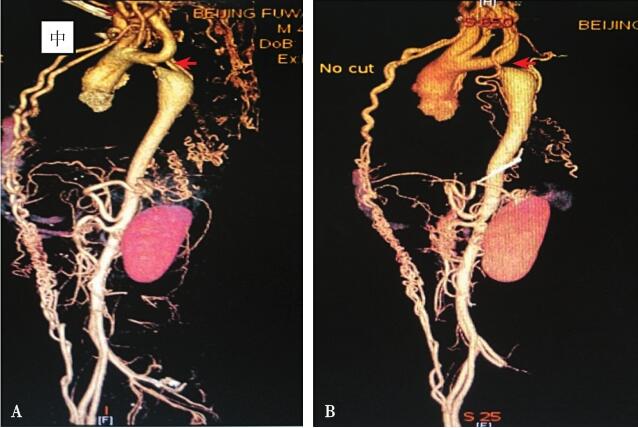
这是一项回顾性队列研究,纳入在单中心随访接受缩窄修复且年龄≥16岁的834例患者。修复时的中位年龄为3岁(下-上四分位数:1个月至15岁),83%通过外科手术进行修复(690/834),17%通过血管成形术/支架植入术(144/834)。与年龄和性别匹配的正常人群进行生存率比较。其他结局包括主动脉弓再介入、主动脉瓣介入、升主动脉介入、以及最近一次随访时的残余/再缩窄和静息高血压。
中位随访27年后(上-下四分位数:18-36),有38例晚期死亡(5%,38/834)。30岁、50岁和70岁的总体生存率分别为99%、88%和65%,与匹配的正常人群相比显著降低(标准化死亡率:3.20,对数秩:p<0.001)。30%的患者(246/834)需要≥1次主动脉弓再介入,13%(111/834)需要主动脉瓣介入和5%(43/834)需要升主动脉介入。50岁时不需要主动脉瓣和升主动脉介入的比例分别为83%和92%,70岁时为53%和81%。最近一次随访时60%(282/474)存在残余/再缩窄(梯度≥25mmHg或修复部位/膈肌比率≤70%),57%(379/661)有静息高血压。
缩窄修复当代成人幸存者的长期生存率显著低于匹配的正常人群,并在第三个10年后加速下降。近60%的患者最终发展为高血压,而约50%的患者在50岁时需要进一步的侵入性心血管治疗。该风险分层数据可以为这种常见的先天性心脏病提供个性化的随访策略。
原始出处:
Melissa G Y Lee. Long-term mortality and cardiovascular burden for adult survivors of coarctation of the aorta. Heart. 28 March 2019.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#主动脉缩窄#
34
#ART#
27
#主动脉#
31
#HEART#
30