Mov Disord:新量表,助力帕金森患者的胃肠道紊乱状态评估
2021-08-08 Freeman MedSci原创
帕金森病胃肠功能紊乱量表是一种新型的疾病特异性自我报告工具,并可定量评估帕金森病患者胃肠功能紊乱特征的存在和严重程度,具有很强的可靠性和有效性。
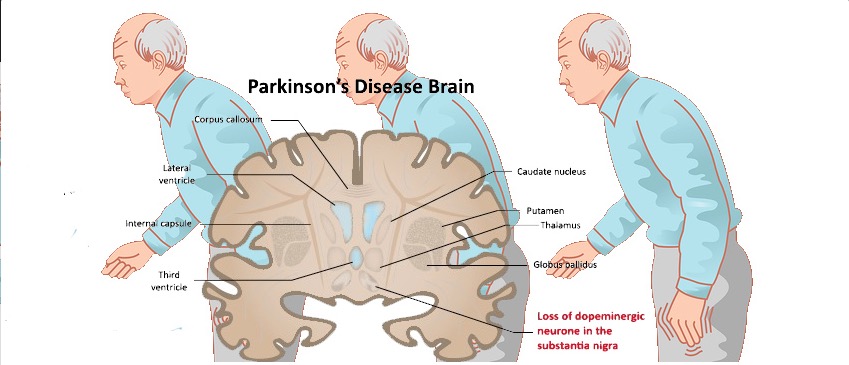
尽管帕金森病(PD)的特点是运动障碍,但它与显著的非运动特征有关,包括胃肠道功能障碍(GID)。便秘是最常见的非运动性帕金森病症状之一,可显著影响患者的生活质量。有便秘的人患帕金森病的风险更大,现在它是帕金森病前兆的一个公认特征。其他胃肠道(GI)特征会随着PD的发展而带来重要的管理挑战:胃排空延迟对营养不良和药物吸收有影响,吞咽困难和唾液流出是吸入性肺炎的风险因素,而吸入性肺炎是PD的一个常见死因。此外,对肠道-大脑轴的研究已经急剧增加,越来越多的证据表明,肠道功能障碍可能在PD的早期发病机制中起作用。
GID的临床评估在很大程度上依赖于自我报告的症状,因此对这些症状进行有力和全面的测量对于这一关键领域的研究至关重要。不幸的是,目前这种评估由于使用不同的技术和心理测量工具以及基于不同的GID标准而受到限制。Knudsen等人在PD文献中发现了10多个便秘定义,这阻碍了对结果的解释和对PD中GID的理解。
评估PD中GID,最广泛使用的量表是一般的非运动症状工具:运动障碍协会统一帕金森病评定量表、帕金森病结果量表-自主神经(SCOPA-AUT)和非运动症状量表(NMSS)。
针对帕金森病GID具体方面的有效心理测量工具包括帕金森病唾液分泌临床量表和吞咽障碍调查表。 虽然其他量表也被使用,但它们并不是为PD人群设计或验证的,也没有涵盖PD中GID的全部临床范围。
此外,现有的心理测量问卷与更客观的便秘、吞咽困难和胃液反流的测量方法只有适度的相关性。使用共同的标准对结果的普及至关重要,目前还没有专门用于PD的心理测量工具反映最近的国际疾病分类(ICD)-1029和罗马IV21标准,这两个标准分别是评估胃肠道疾病和功能性胃肠道疾病病理标准的黄金标准。
同样,目前没有任何工具包括生活方式和已知的重要混杂因素(即饮食、吸烟习惯、运动、胃肠道合并症),这需要通过额外的工具进行评估。
此外,现有量表缺乏分界点,不能进行样本分层或提供与消化道相关的结果测量,以前的研究大多采用中位数或绝对变化来对队列进行分层。
因此,需要一个PD专用工具来评估胃肠道症状,提供对病人分层有用的分界点,并在即将进行的观察性研究和临床试验中促进这些症状的定量。
藉此,剑桥大学的Marta Camacho等人,开发了帕金森病胃肠功能障碍量表(GIDS-PD),并在帕金森病患者和类似年龄的对照组样本中研究其心理测量特性。
他们进行了文献回顾,以制定帕金森病的胃肠功能障碍量表。316名帕金森病患者和55名对照者完成了帕金森病胃肠功能障碍量表、非运动性症状量表、医院焦虑和抑郁量表以及大便的记录。
他们发现,GIS量表,显示出良好的内部一致性(Cronbach's α = 0.82)和测试-回归稳定性( ICCs在0.79和 0.94之间)。
相关性分析支持良好的收敛和发散有效性(convergent and divergent validity)。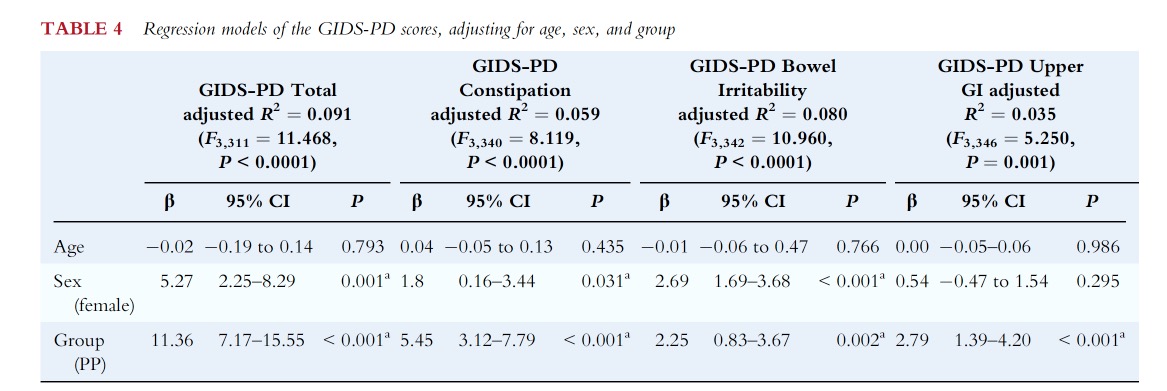
ROC分析表明,GIS量表的临界分值≥9,可以区分有便秘和无便秘的帕金森病患者。
这个研究的重要意义在于发现了:帕金森病胃肠功能紊乱量表是一种新型的疾病特异性自我报告工具,并可定量评估帕金森病患者胃肠功能紊乱特征的存在和严重程度,具有很强的可靠性和有效性。
但可能需要进一步的纵向研究,来证明其在跟踪帕金森病临床队列中胃肠功能紊乱的效用。
点击下载:GIS最新量表.pdf
原文出处:
Camacho M, Greenland JC, Williams‐Gray CH. The Gastrointestinal Dysfunction Scale for Parkinson’s Disease. Mov Disord. Published online June 16, 2021:mds.28675. doi:10.1002/mds.28675
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#Dis#
44
#Disord#
49
可以在临床中试试
65
#胃肠道#
38
弄点积分太难了,费劲
65
可以看看
70
不错
50