诊疗规范丨结缔组织病相关肺动脉高压如何诊治?
2022-04-20 中华医学会风湿病分会 中华医学会风湿病分会
肺高压(PH)是结缔组织病( CTD)的严重并发症之一。越来越受到风湿免疫科医生的重视。
肺高压(PH)是结缔组织病( CTD)的严重并发症之一。其中,第一大类PH,即肺动脉高压(PAH)最为常见,其起病隐匿、临床表现缺乏特异性、早期诊断困难、治疗效果不佳。尽管目前治疗手段已经得到极大的改进,PAH仍然是CTD患者死亡的重要因素之一,因此得到风湿学界越来越多的重视。
近年来,PAH领域研究进展迅速,多项国际及国内高质量临床研究提供更多循证医学证据,诊疗指南也持续更新。本文特摘录发表于中华医学会风湿病学分会的“结缔组织病相关肺动脉高压诊疗规范”相关诊治内容,以助临床参考。
01 CTD-PAH的诊断标准
疑诊CTD-PAH的患者经初步筛查支持PAH诊断后,应尽早完善右心导管(RHC),必要时完善肺功能、肺通气灌注显像、CT肺动脉造影等检查进行准确诊断分类(参见图1)。RHC不仅是确诊PAH的金标准,也是进行鉴别诊断、评估病情和进行相关临床研究必不可少的手段。

图1. CTD-PAH筛查及病情评估流程
根据2015年ESC/ERS指南,PAH的定义为:在海平面、静息状态下,RHC测得肺动脉平均压(mPAP)≥25 mmHg,PAWP≤15mmHg,PVR>3WU。2018年,第6届世界肺动脉高压大会(WSPH)发布PAH新的定义,将mPAP临界值下调,即满足mPAP>20mmHg可诊断为肺动脉高压(PAWP、PVR不变),这使得PAH能够更早得到诊断。2021年的中国肺动脉高压诊断及治疗指南(中华医学会呼吸病学分会肺栓塞与肺血管病学组、中国医师协会呼吸医师分会肺栓塞与肺血管病工作委员会等提出)并没有采纳相关更改,仍以mPAP≥25 mmHg作为诊断标准;但对于CTD-PAH患者而言,mPAP临界值降低可能会利于实现早期筛查、早期干预,建议适当增加筛查频率,密切观察疾病进展程度。但需知,该类患者(mPAP 21~24mmHg)能否在PAH特异性治疗中获益有待进一步临床研究证实。
02 CTD-PAH的治疗原则和目标
CTD-PAH治疗原则是早期、个体化治疗,最大程度的延缓疾病进展、降低器官损害,最终延长患者生存期,提高生活质量,改善预后。治疗目标应是CTD和PAH“双重达标”(图2)。
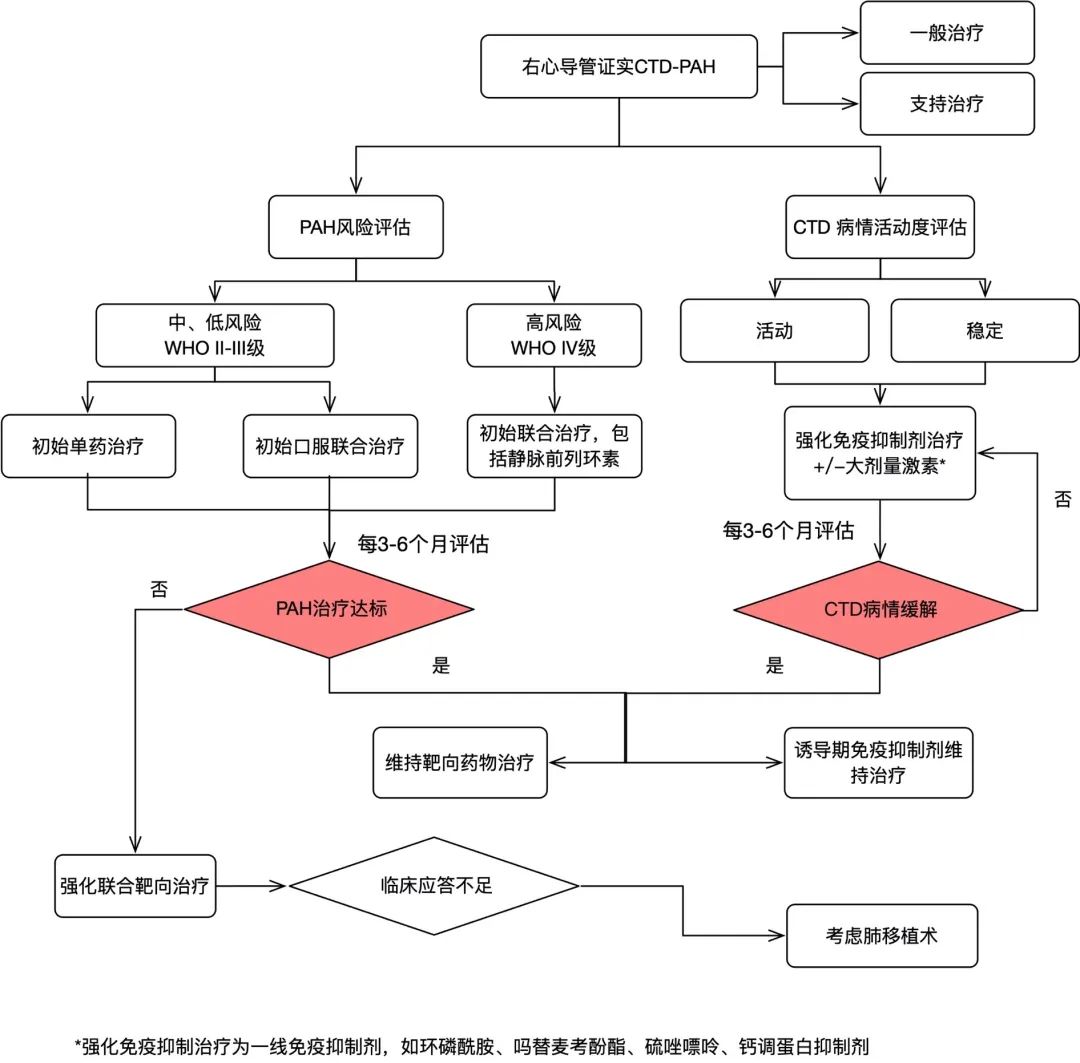
图2. 中国CTD相关PAH诊疗策略
03 CTD-PAH的基础治疗
01利 尿
CTD-PAH患者出现失代偿右心衰竭往往合并水钠潴留,表现为中心静脉压升高、肝淤血、腹水和外周水肿,利尿剂可有效改善上述症状。常用利尿剂包括襻利尿剂和醛固酮受体拮抗剂。应用利尿剂时应监测肾功能和血生化指标,避免出现电解质紊乱和血容量下降引起的肾前性肾功能不全。临床中对容量不足,尤其RHC测定右心房压力偏低,超声心动图提示左心室严重受压且血压偏低的患者,应谨慎使用利尿剂。
02吸氧
有研究证实,对于PAH患者,长期氧疗有助于降低肺动脉平均压力和肺血管阻力,当外周血氧饱和度<91%或动脉血氧分压<60mmHg时建议吸氧,使动脉血气氧分压维持在60mmHg以上。
03地高辛
地高辛可增加心脏收缩力,改善PAH患者心输出量,控制心室率,但长期疗效尚不清楚。心衰程度较重的患者可酌情考虑使用。
04铁剂
铁缺乏在PAH患者中较为普遍,尤其是CTD-PAH患者,其可使CTD-PAH患者运动耐量下降,病死率增加。铁缺乏的病因考虑PAH存在铁代谢障碍,同时长期慢性炎症也是重要原因之一,严重患者会出现缺铁性贫血。建议在随诊过程中常规监测,必要时应用补铁药物纠正。
05抗凝
口服抗凝治疗在CTD-PAH的风险-获益比尚不明确,应根据患者血栓风险程度评估后制定抗凝策略。通常CTD患者合并抗磷脂抗体阳性,或者核素肺通气/灌注显像结果提示存在中、高度可疑肺栓塞等情况,建议口服维生素k拮抗剂药物长期抗凝,国际标准化比值(INR)目标为2.0-3.0之间。新型口服抗凝药在CTD-PAH中的疗效尚不明确。
06钙离子拮抗剂(CCBs)
只有急性血管反应试验阳性的特发性PAH患者才可能从CCBs治疗中获益,而试验阳性的CTD-PAH患者接受CCBs治疗获益情况不明确;如应用CCBs需每3月评估治疗反应,对疗效不佳的患者应尽快转至PAH靶向药物治疗。
04针对CTD的治疗
01治疗目标
应积极追求CTD病情缓解。总体以PGA<1分表示CTD处于临床缓解状态。
以三种常见CTD为例:
①SLE低疾病活动度:SLE活动度评分(SLEDAI-2K)≦4分,BILAG各系统评分为C/D/E级,PGA<1分,强的松剂量每天≦7.5mg,未使用免疫抑制剂。SLE缓解:SLEDAI为0分,PGA<0.5分,仅服用抗疟疾药物。
②pSS低疾病活动度:SS欧洲抗风湿病联盟疾病活动度指数(ESSDAI)<4分。pSS治疗反应目标:ESSDAI分数降低≥3分。
③SSc:虽无确切的活动性评估体系,但短期内无进展性皮肤或肺部纤维化病变或血管病变(指端溃疡、PAH)可作为治疗目标。
02治疗方案
强化免疫抑制治疗有助于CTD-PAH病情改善。应根据CTD类型、疾病活动度、病程、受累器官及严重程度制定个体化的免疫抑制方案。与IPAH相比较,CTD-PAH的治疗更为复杂,在治疗PAH同时还需积极控制CTD病情,进而实现“双重达标”,方能改善远期预后,提高患者生活质量。判断原发病是否活动为治疗的第一步。
①若原发病活动明显、或者有明确的其它重要脏器受累,应根据原发病的治疗原则进行方案制定。
②若原发病存在活动证据(如:SLE患者补体减低、抗ds-DNA明显升高;或pSS患者紫癜明显、IgG升高等),但除PAH之外无其它脏器严重受累,亦应积极免疫抑制治疗。既往研究发现,在SLE、pSS及MCTD-PAH患者群体中,通过大剂量糖皮质激素联合免疫抑制剂诱导缓解治疗可有效地控制PAH。应选择较强的免疫抑制剂如环磷酰胺(CTX)、吗替麦考酚酯(MMF)等。部分患者若原发病活动明显,或处于病程早期,评估相关风险后可酌情加用激素冲击治疗,为其争取“逆转”PAH的希望,建议结合具体病情进行个体化选择。
③若原发病稳定,肺高压仍进展的患者:治疗重心可稍向“靶向治疗”偏倚。原发病方面可维持原激素用量,亦可结合实际情况增加至半或足量激素治疗,但应尽快逐渐减量;免疫抑制剂建议适当强化,因PAH的出现提示原治疗方案强度不足以抑制PAH,结合其病情可强化为CTX、MMF、硫唑嘌呤等。
④原发病及肺高压均稳定:建议采用维持缓解期的治疗方案,即小剂量糖皮质激素及能够长期应用的免疫抑制剂,例如钙调磷酸酶抑制剂(环孢素、他克莫司)、吗替麦考酚酯、硫唑嘌呤、甲氨蝶呤或羟氯喹等药物。
⑤对于SSc-PAH患者,现有的研究都显示激素及免疫抑制剂不能改善患者症状、血流动力学及预后,因此是否加用激素及免疫抑制剂,建议根据SSc疾病分期以及其他脏器受累情况决定。
特别需要指出的是虽然SLE、SS及SSc的疾病活动性评分均未将PAH纳入评估,但不能片面地将PAH完全隔离出来单独评估,应将PAH作为CTD系统受累的一部分进行全面的综合考虑,在临床实践中进行个体化治疗。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#结缔组织#
41
#动脉高压#
47
#结缔组织病#
52
***
69
干货
77
***
69
***
68