J Gastroenterology: 内镜治疗无症状胆管结石的临床结果分析
2019-09-18 不详 MedSci原创
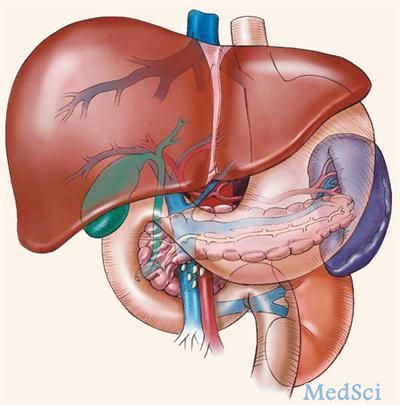
由于腹部影像学检查机会增加,患者偶尔会被诊断出没有任何症状的胆管结石。然而,对无症状胆管结石的管理尚未达成共识。因此,研究人员进行了回顾性纵向队列研究,以根据内镜治疗的情况来调查无症状胆管结石的自然史和临床预后。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#临床结果#
23
#AST#
30
#Gastroenterol#
31
#GAS#
26
#内镜#
28
#内镜治疗#
51
#无症状#
25
#Gastroenterology#
21
#胆管#
24