JCEM:用于评估自身免疫性甲状腺疾病风险和严重性的miRNA标签
2018-01-10 MedSci MedSci原创
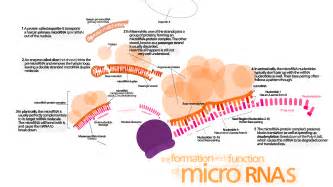
众所周知循环miRNA因为其作为新型生物标记物和治疗靶标的潜在作用,正在成为一个研究热点,然而其在自身免疫性甲状腺疾病(AITD)中所起的作用还未得到充分研究。2018年1月9日在JCEM上发表的一篇文章则通过下一代测序比较AITD患者和对照者甲状腺组织中的miRNA的表达谱,并用qRT-PCR证实,进一步验证其血清样本中的发现。
众所周知循环miRNA因为其作为新型生物标记物和治疗靶标的潜在作用,正在成为一个研究热点,然而其在自身免疫性甲状腺疾病(AITD)中所起的作用还未得到充分研究。2018年1月9日在JCEM上发表的一篇文章则通过下一代测序比较AITD患者和对照者甲状腺组织中的miRNA的表达谱,并用qRT-PCR证实,进一步验证其血清样本中的发现。
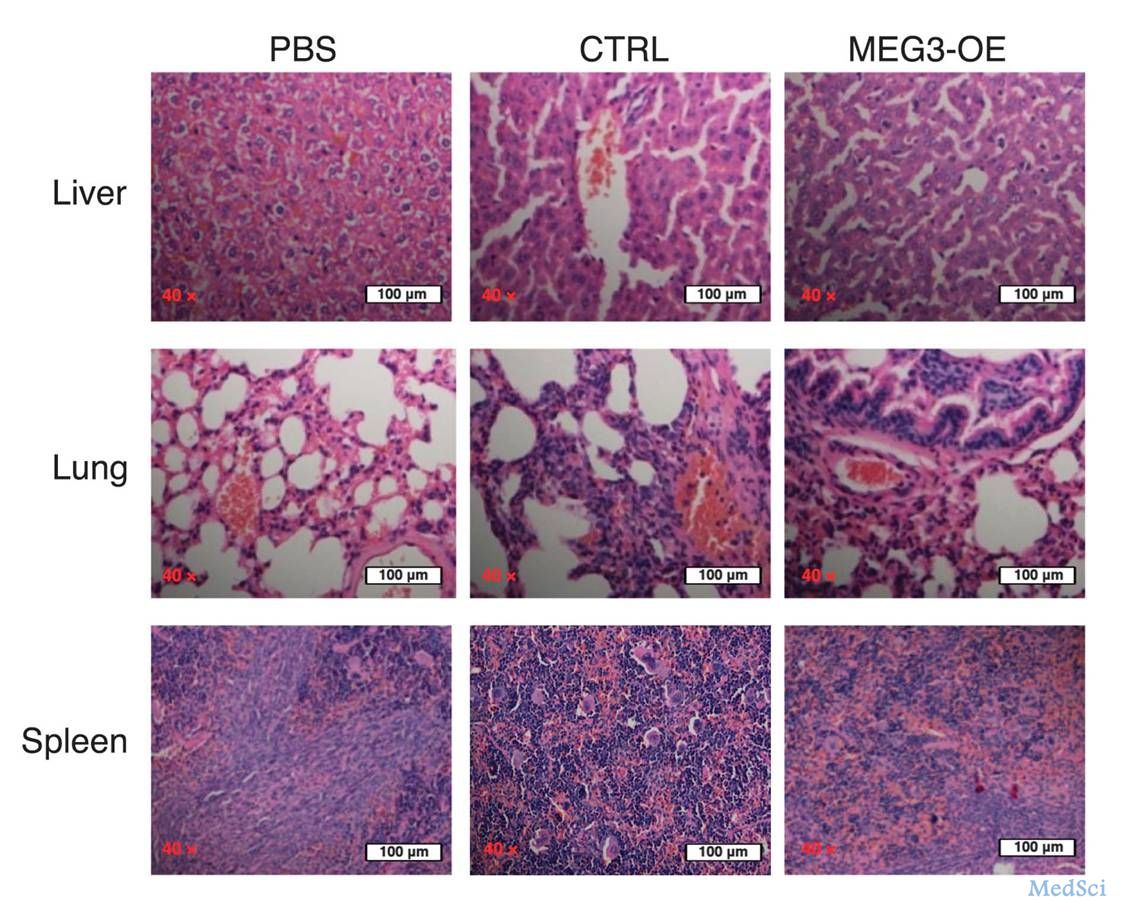
研究人员共采集到20个新鲜冷冻的甲状腺组织(15个来自AITD和5个对照)用于miRNA下一代测序。 qRT-PCR验证试验招募了36份甲状腺样本,58份血清样本在外周血中进一步验证。
研究结果显示先前与相关免疫功能有关的几种miRNA的表达显着失调。具体来说,使用qRT-PCR证实了甲状腺组织中的8种差异性表达的miRNA miR-21-5p,-142-3p,-146a-5p,-146b-5p,-155-5p,-338-5p,-342-5p,-766-3p),其中3个在组织和血清样本中(miR-21-5p,-142-3p和-146a-5p)有相同的行为。除此之外,当这些miRNA的表达与先前与外周血中的AITD相关的另外五种miRNA一起评估时,其中五种(miR-Let7d,-21-5p,-96-5p,-142-3p和-301a-3p)在AITD中显着表达,在GD患者中与疾病的严重程度相关,包括活性眼病、甲状腺肿、较高的抗体滴度和/或较高的复发率。
上述研究表明目前确定了一个血清5-miRNA标签,可能是AITD发展的独立危险因素,也是GD患者临床症状恶化的诱因。
原始出处:
Rebeca Martínez-Hernández.et al. A microRNA signature for evaluation of risk and severity of Autoimmune Thyroid Diseases. J Clin Endocrinol Metab. 2017.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#JCEM#
31
#严重性#
41
#自身免疫性甲状腺疾病#
36
#JCE#
30
#miR#
26
#miRNA#
25
#疾病风险#
22
学习一下谢谢分享
66
^_^^_^^_^^_^^_^
50
学习了.谢谢.
51