Blood:抗CD19 CAR T细胞治疗后病情进展的B-ALL成人患者的干预措施和临床预后
2021-08-26 Nebula MedSci原创
抗CD19 CAR T细胞疗法后病情进展的B-ALL成人患者的总体预后较差
中心点| CAR T细胞治疗后病情进展的B-ALL患者预后较差,仍是未被满足的临床需求;CAR T细胞治疗后病情进展的患者,通过博纳吐单抗、Inotuzumab或再输注CAR T细胞治疗还可获得完全缓解,但缓解持续时间和生存期都有限。
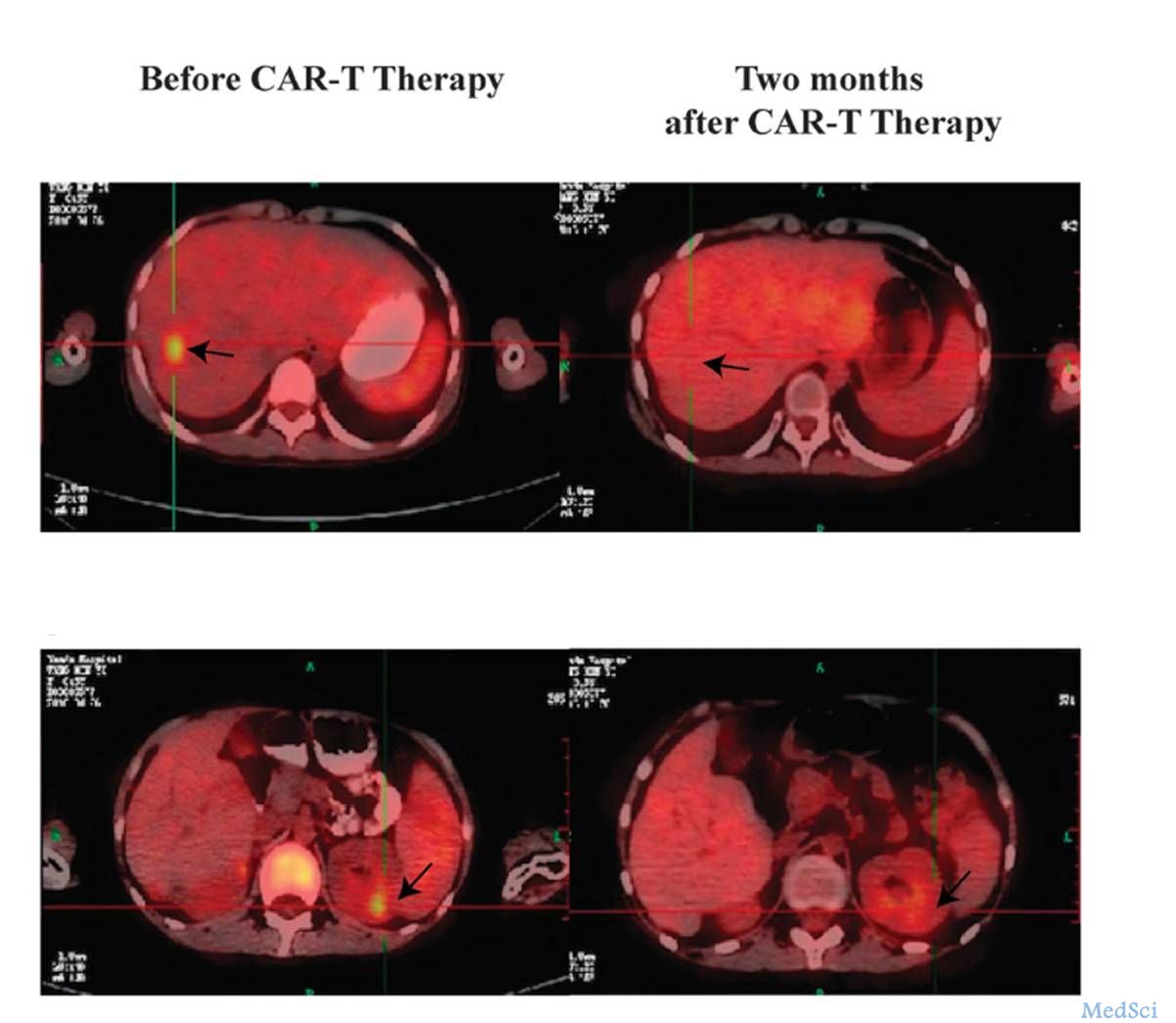
CD19靶向嵌合抗原受体(CAR)T细胞疗法是复发性/难治性B细胞急性淋巴细胞白血病(B-ALL)患者的突破性治疗方法。但是,虽然在CAR T细胞疗法的应用下,初期缓解率高,但大部分B-ALL患者最终还是会发生病情进展。
目前尚无关于CD19 CAR - T细胞治疗后B-ALL成人患者病情进展的自然史、管理和预后结果的详细数据。为补充这方面数据,Wudhikarn等汇报了在其单位接受CD19 CAR T细胞疗法后病情进展的38位B-ALL成人患者的综合数据,报告于近日发表在了《血液》杂志上。
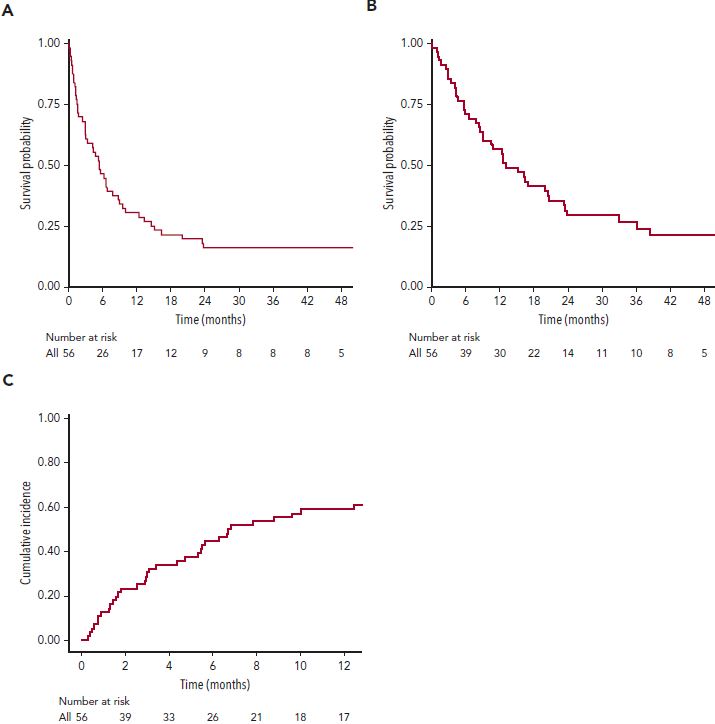
(A)3年无进展生存率;(B)3年总生存率;(C)累积复发率
CAR T细胞治疗后病情进展前的中位时间为7.5个月。3年无进展生存率(EFS)为16.1%(95%CI 8.8-29),3年总生存率为26.6%(95%CI 17-42),一年累积复发率为67.9%(95%CI 53.6-78.6)。CAR T细胞输注时高疾病负荷与CAR T细胞治疗后病情进展的风险显著相关。30位(79%)患者接受了针对CAR T细胞治疗后病情进展的挽救治疗,13位(43%)获得了完全缓解(CR),这13位患者的中位EFS为4.5个月(95%CI 2.1-32.1)。
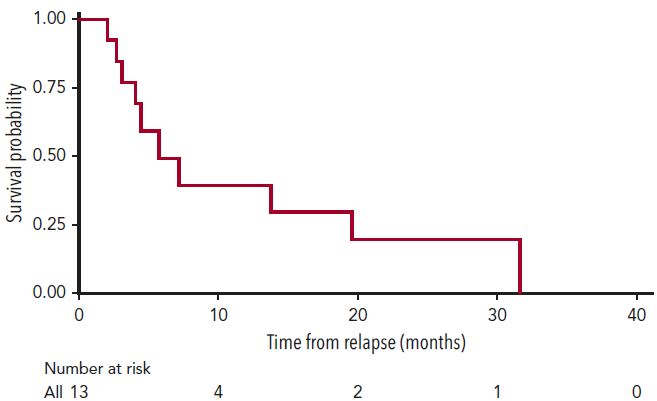
经挽救治疗获得完全缓解的患者的EFS
值得注意的是,12位患者中有7位(58.3%)在CAR T细胞治疗失败后的接受博纳吐单抗和/或Inotuzumab治疗获得了完全缓解。多变量分析显示,CAR T细胞治疗后缓解持续时间长的患者,后续(CAR T细胞疗法后)病情进展后的生存预后也相对较好。
总之,抗CD19 CAR T细胞疗法后病情进展的B-ALL成人患者的总体预后较差,虽然部分患者通过挽救治疗(包括博纳吐单抗、Inotuzumab、再输注CAR T细胞)还可以获得完全缓解。因此,我们需要新的治疗策略来降低B-ALL成人患者经CAR-T细胞治疗后病情进展的风险,并改善这部分患者的预后。
原始出处:
Kitsada Wudhikarn, et al. Interventions and outcomes of adult patients with B-ALL progressing after CD19 chimeric antigen receptor T-cell therapy. Blood (2021) 138 (7): 531–543. https://doi.org/10.1182/blood.2020009515
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#病情#
32
#干预措施#
36
#ALL#
21
#CD19#
46
#B-ALL#
43
#临床预后#
30