JAMA:未行手术干预的无症状严重颈动脉狭窄患者5年内发生缺血性卒中风险为4.7%
2022-05-30 影像小生 MedSci原创
未接受手术干预的患者5年内患同侧颈动脉相关急性缺血性卒中的估计比率为4.7%
无症状重度颈动脉狭窄患者不进行手术干预的卒中发生率是多少?JAMA刊发回顾性队列研究,该研究包括了3737名参与者,他们在2008年至2012年期间发现了70%至99%的无症状颈动脉狭窄,并在2019年进行了随访,他们没有接受手术干预。5年内同侧颈动脉相关急性缺血性卒中的估计发生率为4.7%。这些发现可以为无症状严重颈动脉狭窄患者的治疗决策提供参考。
自1995年和2010年发表若干随机临床试验以来,无症状颈动脉疾病的最佳治疗已涉及若干随机临床试验的选择性。从那时起,药物治疗取得了进展,报道显示单独药物治疗的结果有所改善,这引发了对无症状患者干预预防中风的绝对增益的质疑。未行手术血管重建术的无症状颈动脉疾病的卒中风险难以确定,因为数据来源仅限于非手术组临床试验、罕见的前瞻性研究或较小的干预基础研究。此外,考虑到这些研究对象的年龄,它们不能解释最近在减少人群心血管风险方面的进展。
Robert W. Chang等在JAMA发表研究文章,目的是在一个更现代、种族和民族多样化的社区人群中,评估未接受手术干预的无症状严重颈动脉狭窄患者药物治疗的的卒中结局。
该研究为回顾性队列研究,包括 3737 名在 2008 年至 2012 年间被诊断为无症状严重 (70%-99%) 颈动脉狭窄且在前 6 个月内未进行过干预或同侧神经系统事件的成年参与者。参与者接受了随访。影像学诊断无症状的颈动脉狭窄程度为70%~99%。主要评估参数为同侧颈动脉相关性急性缺血性卒中的发生率。
该研究发现
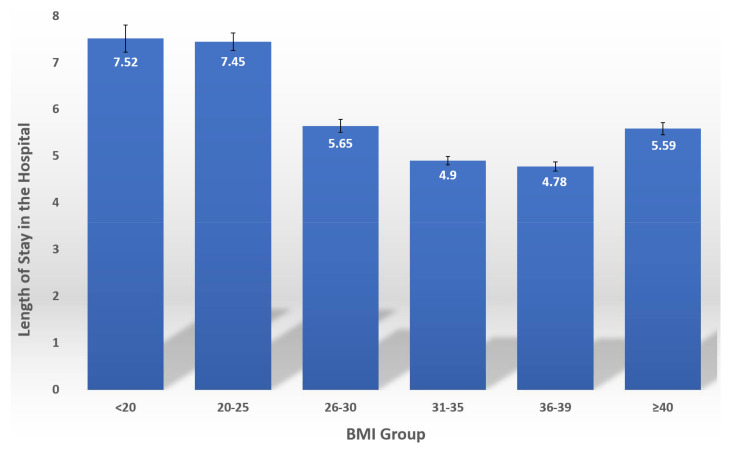
表2. 卒中和全因死亡率(每条动脉)
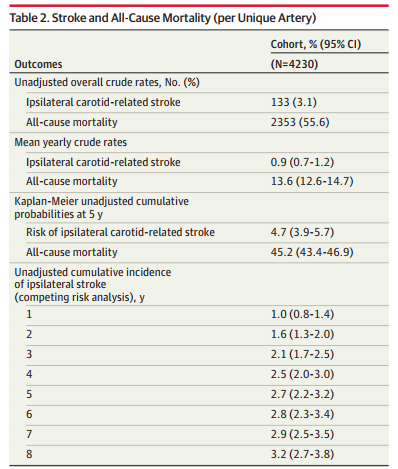
在 94822 名影像学检查合格的患者中,3737 名患者中的 4230 支动脉(平均年龄 73.8 [SD 9.5 岁];57.4% 为男性)符合选择标准,包括 2314 名从未接受过干预的患者中的 2539 支动脉。该队列的平均随访时间为 4.1 年(标准差 3.6 年)。
在任何干预之前,有 133 例同侧卒中,平均年卒中发生率为 0.9%(95% 置信区间 [CI],0.7%-1.2%)。Kaplan-Meier 估计 5 年同侧卒中的发生率为 4.7%(95% CI,3.9%-5.7%)。
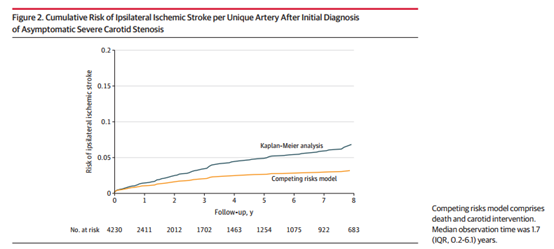
图2. 初次诊断无症状严重颈动脉狭窄后,每条唯一动脉同侧缺血性卒中的累积风险
总之,在一个社区为基础的无症状重度颈动脉狭窄患者队列中,未接受手术干预的患者5年内患同侧颈动脉相关急性缺血性卒中的估计比率为4.7%。这些发现可以为无症状严重颈动脉狭窄患者的手术和药物治疗提供决策依据。
原文出处
Chang RW, Tucker LY, Rothenberg KA, et al. Incidence of Ischemic Stroke in Patients With Asymptomatic Severe Carotid Stenosis Without Surgical Intervention. JAMA. 2022;327(20):1974-1982. doi:10.1001/jama.2022.4835
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#缺血性卒#
41
#缺血性#
0
#颈动脉#
40
#手术干预#
35
学习
48
#卒中风险#
34
#无症状#
42
#动脉狭窄#
42
JAMA上文章都是顶级的,谢谢梅斯及时上新
37