European Radiology:究竟哪些肝炎患者需要做EOB-MRI检查?这个血清学指标你一定要知道!
2022-05-01 shaosai MedSci原创
非血管性低信号结节(NHHNs)是通过普美显增强磁共振成像(EOB-MRI)检测出的一类肝脏结节。
肝细胞癌(HCC)是目前世界上最常见的癌症相关死亡原因之一,其中HCV感染是HCC的一个主要原因。HCC患者的预后在很大程度上取决于早期发现和治疗。对高危患者进行HCC监测与早期发现、进行根治性治疗和更好的总生存率相关。因此,有效的HCC监测和识别有HCC风险的患者对于改善预后非常重要。
非血管性低信号结节(NHHNs)是通过普美显增强磁共振成像(EOB-MRI)检测出的一类肝脏结节。在肝胆期,NHHNs相对于肝实质显示为较低信号,但在动脉期呈弱强化。以前的研究报告指出,NHHNs在长期随访过程中,随着其体积的增长很有可能出现血管增粗的现象。血管过多的结节通常具有HCC的影像学特征,包括廓清和包膜强化,常提示发展为典型HCC。因此,NHHN的存在是HCC发展的一个强有力的风险因素。因此,HCC的高风险患者可以通过NHHN的存在来识别。
据报道,FIB-4指数值与HCV感染患者的HCC发展有关。血清甲胎蛋白(AFP)是HCC的一个肿瘤标志物。最近的一项研究报告说,HCC患者的AFP水平在确诊HCC前很久就已经升高。另一项研究报告说,血清中WFA+-M2BP的升高与HCV感染患者HCC的高发生率有关。
近日,发表在European Radiology杂志的一项研究评估了HCC潜在的基于实验室的风险因素与HCV感染患者中NHHNs的存在之间的关系,这可协助临床识别出有高风险NHHNs存在的患者以进行进一步的EOB-MRI检查以明确诊断。

本研究对481名接受EOB-MRI检查的HCV感染和无HCC病史的患者测量了三种血清标志物,即甲胎蛋白(AFP)、FIB-4指数和M2BPGi,并研究了这些血清标志物水平与NHHNs的存在之间的关联。
所有三个标志物都与NHHNs的存在有关。M2BPGi比AFP和FBB-4指数更准确地预测NHHNs的存在;M2BPGi的ROC曲线下面积最高。多变量分析确定男性和高M2BPGi是与NHHNs存在相关的因素。当患者按肝脏纤维化程度分层时,M2BPGi随着纤维化的进展而增加。此外,在纤维化程度相似的患者中,M2BPGi较高(COI>3.46)的患者更容易发现NHHNs。
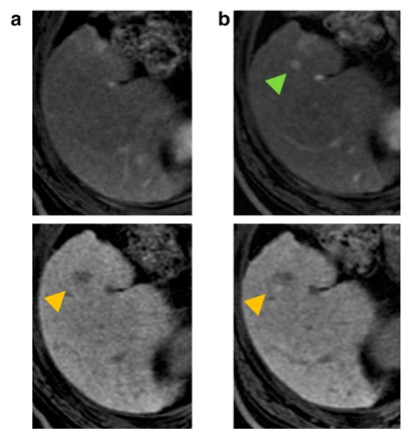
图 EOB-MRI图像上的非血管性低信号结节(NHHNs)向血管性肝癌(HCC)的转变。上图为EOB-MRI的早期动脉期;下图为EOB-MRI的肝胆期。(a)NHHN和(b)NHHN的高血管化
本研究显示,在慢性HCV感染患者中,NHHNs的存在与M2BPGi、AFP和FIB-4指数值之间存在相关性。特别是,M2BPGi与NHHNs的存在独立相关,是确定EOB-MRI合适人选的一个潜在血清学指标。
原文出处:
Hidenori Toyoda,Satoshi Yasuda,Shohei Shiota,et al.Identification of the suitable candidates for EOB-MRI with the high risk of the presence of non-hypervascular hypointense nodules in patients with HCV infection.DOI:10.1007/s00330-022-08570-4
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#PE#
40
#肝炎患者#
41
#MRI检查#
39
#血清学#
37