European Radiology:MRE在评估HCC微血管侵犯中的应用
2022-04-18 shaosai MedSci原创
MR弹性成像(MRE)是一项成熟的技术,在检测和分期肝脏纤维化方面具有很高的诊断性能,同时在评估恶性肿瘤方面也有新的作用。
 肝细胞癌(HCC)是全世界范围内第五大最常见的恶性肿瘤,也是与癌症相关的第二大死亡原因。肝脏切除术是目前治疗HCC最有效、最常用的术式选择。然而,据报道,HCC的术后5年复发率高达70%,大大缩短了生存时间。微血管侵犯(MVI)是肿瘤侵袭性的指标,是HCC患者肝切除后复发和预后不良的重要独立预测因素。因此,术前预测MVI对于决定患者的最佳临床治疗方案至关重要。然而,与大血管侵犯不同的是,大血管侵犯在术前影像中是可见的,而MVI只能通过术后组织病理进行诊断。因此开发一种无创的方法来预测术前MVI的存在具有相当的临床价值。
肝细胞癌(HCC)是全世界范围内第五大最常见的恶性肿瘤,也是与癌症相关的第二大死亡原因。肝脏切除术是目前治疗HCC最有效、最常用的术式选择。然而,据报道,HCC的术后5年复发率高达70%,大大缩短了生存时间。微血管侵犯(MVI)是肿瘤侵袭性的指标,是HCC患者肝切除后复发和预后不良的重要独立预测因素。因此,术前预测MVI对于决定患者的最佳临床治疗方案至关重要。然而,与大血管侵犯不同的是,大血管侵犯在术前影像中是可见的,而MVI只能通过术后组织病理进行诊断。因此开发一种无创的方法来预测术前MVI的存在具有相当的临床价值。
到目前为止,许多学者通过CT或MRI的影像学特征(如肿瘤边缘、动脉边缘增强或肝胆期的瘤周低信号),试图在术前影像学图像上识别MVI。然而,在评估这些影像特征时,即使是有经验的放射科医生也有很高的观察者间差异,因此导致临床实践中的争议不断。
MR弹性成像(MRE)是一项成熟的技术,在检测和分期肝脏纤维化方面具有很高的诊断性能,同时在评估恶性肿瘤方面也有新的作用。以前的一些MRI研究也表明,MRE可以应用于HCC患者的检测和定性、治疗反应的预测以及治疗反应的监测。最近,一项基于MRE的技术,即 "滑移界面成像"(SII),利用剪切应变图对脑部肿瘤的瘤周组织粘连程度进行了非侵入性的量化,可对具有高风险的手术并发症和手术侵袭性的患者进行识别。
近日,发表在European Radiology杂志的一项研究在病理证实的HCC患者中使用基于MRE的剪切应变图谱作为生物标志物对肿瘤-肝脏界面的特征进行识别,进一步实现术前MVI的无创性评估。
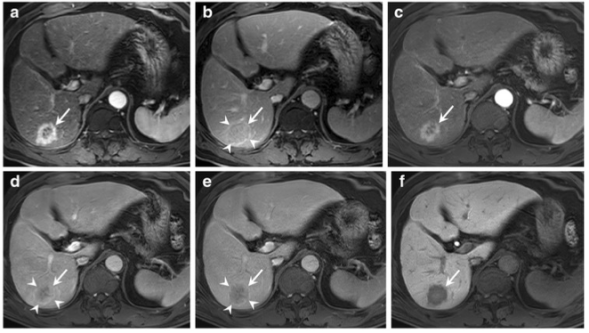
本研究于2016年12月至2019年10月期间,对59名经组织病理学证实的HCC患者进行了常规60Hz MRE检查(+/-MVI,n = 34/25),其中一个亚组包括29/59名患者(+/-MVI,n = 16/13),同时也接受了40和30Hz MRE检查。计算八面体剪切应变(OSS)图,并记录低剪切应变的瘤周界面长度的百分比(即低剪切应变长度,pLSL,%)。对于OSS-pLSL,分别使用MVI(+)组和MVI(-)组之间的差异和不同MRE频率下的诊断性能,用Mann-Whitney检验和受试者工作特性曲线下的面积(AUC)进行分析。
在三个频率下,MVI(+)组的瘤周OSS-pLSL明显高于MVI(-)组(均为P<0.01)。在所有的频率组中,预测MVI的瘤周OSS-pLSL的AUC是良好/优秀的(60-Hz。0.73(n = 59)/0.80(n = 29);40-Hz。0.84;30-Hz。0.90). 在进一步分析所有频率的29个病例时,AUCs没有明显差异。随着频率从60-Hz下降,OSS的特异性在40-Hz增加(53.8-61.5%),在30-Hz进一步增加(53.8-76.9%),而在较低的频率下,敏感性仍然很高(100.0-93.8%)(所有P>0.05)。

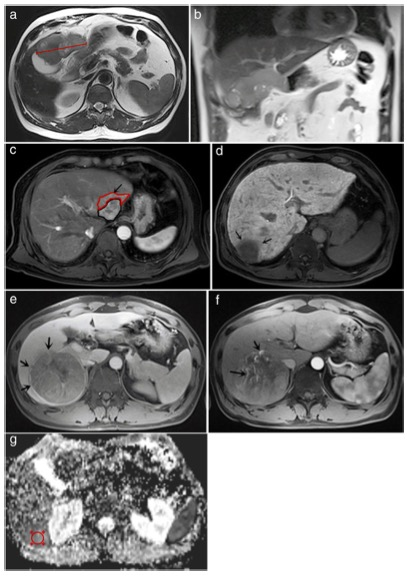
图 a 肿瘤ROI和瘤周肝实质ROI的叠加MRE幅值图像。 b 肿瘤-肝实质接触的实际长度(绿线,62.37mm)。 c 高剪切应变界面(黄色箭头)和低剪切应变界面(白色箭头)的OSS图。 d 低剪切应变肿瘤-肝实质界面的实际长度(白线,8.57mm)
本研究表明,基于MRE的剪切应变图可成为评估HCC患者肿瘤-肝脏界面状态的影像学指标,并可在术前无创地预测MVI的存在。
原文出处:
Mengsi Li,Ziying Yin,Bing Hu,et al.MR Elastography-Based Shear Strain Mapping for Assessment of Microvascular Invasion in Hepatocellular Carcinoma.DOI:10.1007/s00330-022-08578-w
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#MRE#
36
#PE#
36
nice,学习了
42
#HCC#
49
#微血管#
42