NPJ Vaccines:意外之喜!结核疫苗竟能治疗糖尿病,效果可长达 8 年
2018-06-28 佚名 药明康德
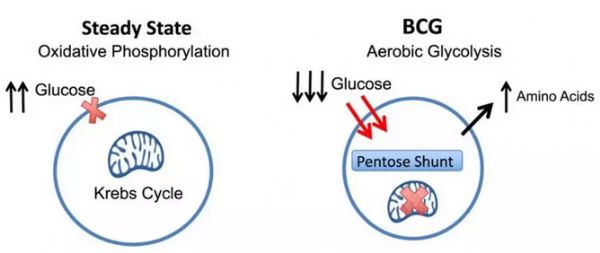
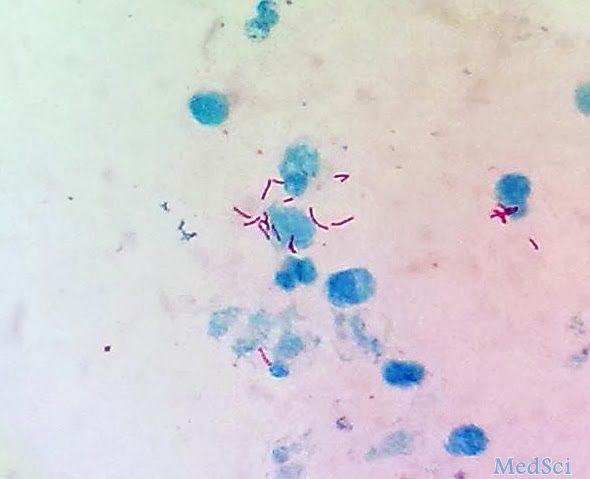
近日,美国麻省总医院(MGH)的研究人员发现 2 剂结核病疫苗卡介苗(BCG)可以将糖尿病患者血糖恢复到接近正常水平,并保持最长达八年时间,同时他们也为这一现象提出了解释。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CIN#
34
#结核#
33
#ACC#
32
学习了谢谢分享
42
伟大的科学家
47
学习了谢谢分享
52