先天性单侧肺静脉闭锁的胸部影像特征
2020-05-20 郭艺帆 何承斌 程建敏 国际医学放射学杂志
单侧肺静脉闭锁(unilateral pulmonary vein atresia,UPVA)是一种罕见的胚胎发育缺陷导致的肺静脉完全闭塞畸形。临床上常以儿童和婴幼儿期肺炎反复发作和咯血为主要表现,部
单侧肺静脉闭锁(unilateral pulmonary vein atresia,UPVA)是一种罕见的胚胎发育缺陷导致的肺静脉完全闭塞畸形。临床上常以儿童和婴幼儿期肺炎反复发作和咯血为主要表现,部分患儿可无明显症状直至成年才被发现。本病主要的诊断手段是CT血管成像(CTA)和数字减影血管造影(DSA),但临床对拟诊肺炎或表现咯血的患儿,往往仅行单纯胸部平片或CT平扫检查,故极易漏诊。本文报道2例UPVA的胸部影像特征,并结合文献进行复习,以期提高对本病的认识。
1.病例1
1.1临床资料
患儿男,2岁。因“咳嗽1个月,发热3d”于2008年12月入院。1个月前无明显诱因出现咳嗽,初发热1次,40℃,我院门诊拟诊“急性上呼吸道感染”,予抗炎、对症处理后,体温即降至正常,但咳嗽持续。近3天患儿出现发热伴呕吐1次,胸部CT拟诊肺炎。
入院查体:体温38.6℃(肛温),呼吸38次/min,呼吸尚平稳,无口唇发绀,双肺呼吸音粗,右肺呼吸音较左肺低,未闻及干湿啰音。支气管镜检查:气管及支气管管腔通畅,右侧各支气管黏膜明显充血水肿,黏膜粗糙,可见纵行皱褶,右上叶为著,表面覆有较多黏稠分泌物。灌洗液培养:金黄色葡萄球菌。尿常规:白细胞(镜检)1~4/高倍,余正常。红细胞沉降率51mm/h。余实验室检查结果未见异常。
1.2设备与方法
1.2.1X线检查
采用德国Siemens YsioDR机进行立位胸部后前位摄片,管电压50kV,管电流采用自动管电流调节技术。
1.2.2CT检查
采用荷兰Philips Brilliance(iCT)256层螺旋CT扫描设备进行胸部平扫及增强检查。准直0.625mm,FOV250mm×250mm,管电压80kV,管电流100mA。平扫:层厚5.00mm,层间距5.00mm;CTA:层厚0.90mm,层间距0.45mm。增强扫描经肘静脉注射对比剂碘普罗胺(含碘370mg/mL)20mL,注射流率1.8mL/s,对比剂注射后追加生理盐水15mL冲管。使用团注追踪技术,将兴趣区(ROI)放在肺野,当右心室成像浓密而左心房、左心室开始浅淡显示时启动扫描。
1.3影像表现
1.3.1胸部平片
右侧胸廓较左侧略小,纵隔轻度右偏,右肺透亮度稍减低,肺纹理模糊,水平裂、斜裂增厚,右肺可见斑片状模糊影(图1A)。结合胸部透视呼吸下出现纵隔摆动,拟诊支气管异物,建议CT进一步检查。
1.3.2胸部CT平扫
气管支气管通畅;右肺小叶间隔明显增厚,呈网格状改变,以肺外周部分明显,胸膜下区多发小楔形条片状影;左肺正常(图1B)。右肺门、纵隔区见软组织密度团块影(34mm×40mm),其肺侧缘呈现沿支气管血管束的尖状突起(图1C)。
1.3.3胸主动脉CTA
右肺动脉管径变细,肺内分支减少;右肺门周围可见增粗、迂曲的支气管动脉。左心房之右侧缘光滑,没有与之相连的右肺静脉,其他处无成形肺静脉异位引流(图1D、1E)。右肺门、纵隔区软组织团块影于静脉期呈明显丛状强化(CT值178HU),与上腔静脉和扩张的奇静脉联系紧密(图1F)。
1.3.4核素扫描
提示右肺灌注缺失,左肺灌注正常(图1G)。

图1 患儿男,2岁,UPVA。A图为胸部平片影像。B、C图为胸部CT平扫影像。D-F图为胸主动脉CTA影像。G图为核素扫描显像,右肺灌注缺失,左肺灌注正常。
1.3.5心脏超声检查
左心增大,二尖瓣轻度反流。
1.4治疗与随访
患儿肺炎首次入院后未接受手术治疗,出院后门诊随访;2009年8月及2010年1月皆因“肺炎”再次住院治疗,好转出院;2010年1月—2017年10月患儿未出现肺部感染情况。
2.病例2
2.1临床资料
患儿男,8岁。因“咳嗽半月余”于2017年9月入院。患儿半月前无明显诱因出现咳嗽,阵发性,较剧烈,咳黄色痰。当时胸片示右肺弥漫性斑片状阴影,心影右移;胸部CT示右肺网状、蜂窝状改变,左肺增大,心脏右移。考虑间质性肺炎。
入院查体:体温36.7℃(耳),呼吸28次/min,呼吸平稳,无口唇发绀,双肺呼吸音粗,对称,未闻及干湿啰音。支气管镜检查:气管管腔通畅,隆突锐利。各支气管黏膜稍充血水肿,表面覆有少量分泌物,右肺各支气管黏膜表面可见较多条索状红色黏膜充血带(图2)。实验室检查未见明显异常。

图2 患儿男,8岁,UPVA。支气管镜检查可见右支气管黏膜表面见较多条索状红色黏膜充血带(系本病支气管镜检查的特征表现)。
2.2设备与方法
CT平扫及CTA检查均采用美国GE Optima66064层螺旋CT扫描设备。准直0.625mm,FOV250mm×250mm,管电压80kV,管电流采用自动管电流调节技术。平扫:层厚5.00mm,层间距5.00mm;CTA:层厚1.25mm,层间距0.625mm。增强扫描经肘静脉注射对比剂碘普罗胺(含碘370mg/mL)45mL,注射流率1.8mL/s,对比剂注射后追加生理盐水30mL冲管。使用团注追踪技术,将ROI放在肺野,当右心室显示浓密而左心房、左心室开始浅淡成像时启动扫描。
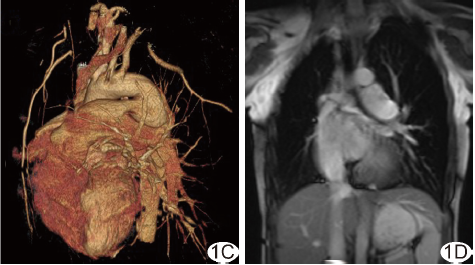
2.3影像表现
胸主动脉CTA显示气管支气管通畅;右肺小叶间隔呈网格状增厚,胸膜下区见明显多发壁菲薄的蜂窝状透亮影(图3A)。右肺动脉管径变细,肺内血管纹理纤细,右支气管动脉增粗、迂曲;左心房之右侧缘光滑,没有与之相连的右肺静脉,其他处无成形肺静脉异位引流(图3B、3C);右侧肺门、纵隔区软组织团块影于静脉期呈丛状强化,其肺侧缘呈现沿支气管血管束的尖状突起(图3D)。
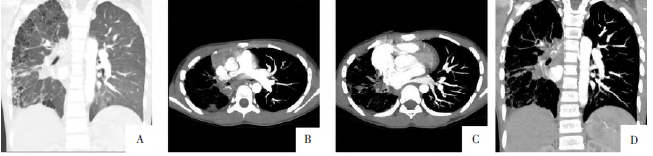
图3 同图2病例。A图为胸部平扫冠状面重组影像。B、C图为胸主动脉横断面CTA影像。D图为胸主动脉冠状面CTA影像。
2.4治疗
患儿经治疗后无反复肺炎、咯血,一般情况好,经儿童心胸外科专家会诊不支持手术,建议门诊随访。
3.讨论
3.1相关胚胎学与临床特点
UPVA的发病机制至今仍不明确。有研究[4,6-7]发现,UPVA系胚胎发育3个月时,与原始肺静脉相连接的体静脉退化消失之后若出现肺静脉或共同腔闭锁,则单或双肺静脉回血不能引入体静脉系统,也不能回归左心房,因而形成UPVA或肺静脉共同腔闭锁。后者患儿常表现为出生后立刻出现进行性心力衰竭及呼吸困难,胸部CT表现为新生儿两肺弥漫性间质淋巴管扩张影,若不立刻行肺静脉矫正术患儿将很快死亡。UPVA的症状及体征缺乏特异性,临床诊断困难,主要表现为反复肺炎或者咯血。约50%患儿合并心脏畸形或异位肺静脉引流,本组2例均没有合并先天性心脏病,支气管镜检查均表现为黏膜静脉曲张,有条索状外观(图2)。这与Tissot等报道的支气管镜检查结果一致。临床上支气管镜下若发现类似表现,需高度警惕UPVA。
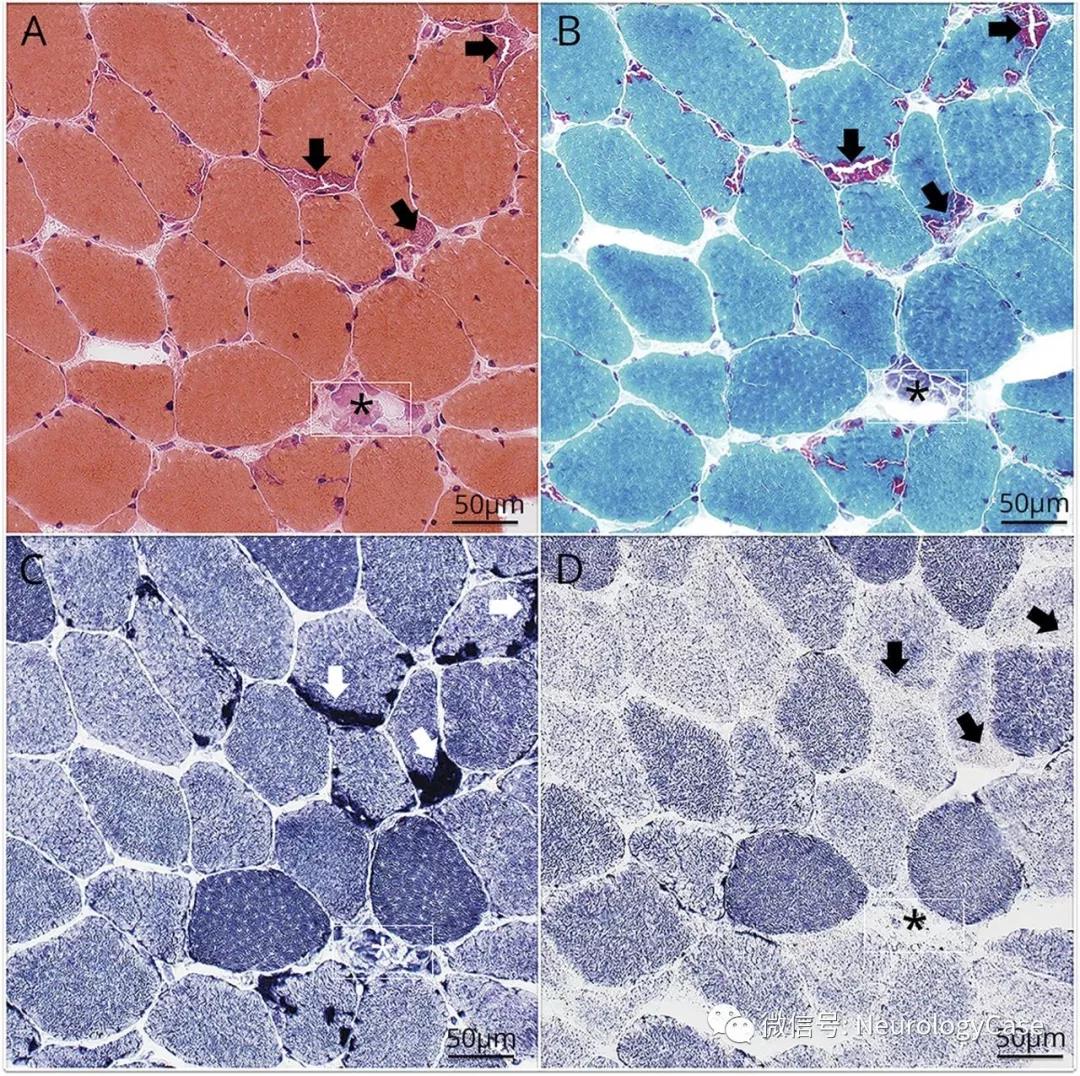
3.2影像诊断及病理基础
UPTA病理改变主要为涉及的肺静脉闭锁、侧支静脉淤滞、慢性肺间质水肿、肺静脉梗死和反复继发感染。Heyneman等报道2例UPVA手术病理发现患侧肺静脉发育不良,肺静脉管壁增厚、硬化甚至管腔闭塞,同侧胸腔和纵隔的侧支静脉管开放;外周静脉和小静脉压力非常高。本研究的2例患儿胸部均表现为单侧肺弥漫间质性纤维化影像。病例1患侧肺全肺弥漫性网格状肺间质增厚,病例2胸膜下区多发蜂窝肺改变。由于UPVA外周静脉和小静脉压力非常高,过多的组织液被挤入淋巴管,导致淋巴管扩张及间质腔的水肿和细胞浸润。肺间质逐渐随成纤维细胞的大量浸润而转变为纤维组织,使原来的组织结构完全变形并失去弹性;病变部位细小支气管牵拉扭曲,导致管腔扩张或狭窄,远侧呼吸性支气管囊状扩张或部分代偿性扩张,或融合成较大的囊泡。
此影像可酷似肺部感染,若不熟悉且仅以影像改变评估“间质性肺炎”吸收情况(如病例1的胸片检查3年均无“肺炎”消退迹象),则极易导致临床抗生素的滥用。UPVA患儿的患侧肺血不能回流左房,且无直接回流的肺静脉显示,而主要通过侧支静脉及淋巴系统回流。
本研究2例患儿的胸部CT平扫均发现患侧肺门、纵隔区软组织影;增强检查纵隔软组织于静脉期明显强化,且强化程度与静脉相仿。Heyneman等利用MRI发现UPVA患儿纵隔软组织内异常流空的血管影,认为该纵隔软组织是脉管系统。因此,患侧纵隔内软组织应是纵隔内静脉和淋巴系统长期接受“超负荷”血流的影像表现。该表现应注意与淋巴结结核病、结节病和淋巴瘤等疾病鉴别,但上述疾病难以解释单侧胸廓变小,纵隔向患侧偏移、单侧慢性间质性肺疾病等影像表现。
此外,本组患侧肺动脉均变细,核素扫描出现无灌注的“矛盾现象”,即有肺动脉供血而无核素扫描灌注。该现象是由于肺弥漫性间质病变使肺弥散功能降低,通气/血流比率明显异常。Firdouse等利用超声多普勒检查发现患侧肺动脉于舒张期有明显的反流,反流由患侧肺动脉流至对侧肺动脉,提示患侧肺血管阻力高。
UPVA患儿行肺动脉成像检查可发现注入的对比剂绝大部分优先进入正常侧肺动脉,由正常侧肺静脉回流;而患侧肺动脉常较小,对比剂流入缓慢。患侧肺静脉系统闭锁,对比剂无正常途径回流至左房,而是经由一些迂曲的毛细血管网与奇静脉沟通。由于患侧肺所接受的右心室泵出血量减少,周而复始的循环影响了肺动脉的发育,导致患侧肺的营养供给下降及间质纤维化,病侧肺因此萎缩,故UPVA患儿在胸部影像上表现为胸廓变小,心脏向患侧偏移,甚至可在透视下见到纵隔摆动。
结合本研究2例及既往报道案例的影像资料,当患儿胸部平片和CT平扫同时具有以下表现时,高度提示UPVA:①单侧肺病变;②患侧胸廓变小,纵隔向患侧偏移,但未见支气管阻塞或空气滞留;③患侧肺弥漫的网格状肺间质增厚;④患侧肺门、纵隔区延伸的软组织团块影,其肺侧缘呈现沿支气管血管束的尖状突起。其中④作为UPVA的特征性影像表现并未在以往文献中专门描述,具备上述表现须进一步行CTA检查。
原始出处:
郭艺帆,何承斌,程建敏,董锋雷,陈博.先天性单侧肺静脉闭锁的胸部影像特征[J].国际医学放射学杂志,2019(01):94-98.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#肺静脉闭锁#
32
#静脉#
38
#先天性#
29
好棒
76
学习了
79