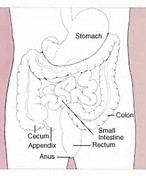
结肠直肠癌是全球第四大癌症致死的相关原因。
关于肿瘤发生在线报道的新发现揭示了IGPR-1如何有助于结肠肿瘤生长和耐药性。
为了生长和生存,正常细胞需要附着于细胞外基质(ECM)上。然而,癌细胞通常会绕过这个步骤,而是直接依靠细胞-细胞粘附进行存活和生长。通过在结肠癌肿瘤中操纵IGPR-1表达,科学家们发现IGPR-1在促进肿瘤细胞(细胞粘附在结肠癌中)起到关键作用。研究人员希望为结肠癌患者提出新的治疗策略。
波士顿大学医学院病理与实验室医学副教授NaderRahimi博士解释说:“我们证明IGPR-1促进肿瘤细胞粘附刺激细胞培养和实验模型中的肿瘤生长。通过特异性阻断抗体和shRNA阻断IGPR-1,抑制肿瘤生长,表明靶向IGPR-1可治疗结肠直肠癌”。
研究人员还证实,IGPR-1决定了肿瘤细胞对化疗药物多柔比星/阿霉素的敏感性,并确定了IGPR-1对结肠癌耐药性的作用机制,这是治疗这种癌症的主要挑战。.
原始出处:
N Woolf, B E Pearson, P A Bondzie1, et.al. Targeting tumor multicellular aggregation through IGPR-1 inhibits colon cancer growth and improves chemotherapy. Oncogenesis
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Gene#
32
非常好的文章!
64
#Oncogene#
38
文章很好.值得分享
51
继续学习中谢谢
64
学习了谢谢分享
64
学习了.谢谢分享
59