2021年8月25日,百时美施贵宝于近日宣布,美国食品药品监督管理局(FDA)批准欧狄沃(纳武利尤单抗)每两周一次240 mg或每四周一次480 mg(静脉注射)方案用于根治性切除术后高复发风险的尿路上皮癌(UC)患者的辅助治疗,且无论患者此前是否接受新辅助化疗、淋巴结受累或PD-L1表达状态。该批准是基于III期临床研究CheckMate -274的结果,该研究旨在评估欧狄沃240 mg(n=353)对比安慰剂(n=356)的疗效与安全性1。此次申请由FDA根据实时肿瘤审评(RTOR)试点项目下进行审评。RTOR旨在确保能尽早为患者提供安全有效的治疗手段2。
尿路上皮癌(UC)最常起源于膀胱内侧的细胞,是美国成年人中最常见的膀胱癌类型。每年有81000例新诊断膀胱癌病例,其中大多数属于尿路上皮癌。除了膀胱,尿路上皮癌也可发生在泌尿道的其他部位,包括输尿管和肾盂。虽然尿路上皮癌可被早期诊断,但其复发率和疾病进展率较高。根据诊断时疾病的分期和其他因素,其生存率也有所不同。对于转移性尿路上皮癌患者,预后往往较差。
CheckMate -274是一项随机、双盲、安慰剂对照、多中心的临床研究,旨在评估欧狄沃作为辅助治疗对膀胱或上尿路尿路上皮癌(UC)根治性切除术后高复发风险患者的疗效。高风险尿路上皮癌患者的病理分期定义标准为:接受过新辅助顺铂化疗,分期为ypT2-ypT4a或ypN+的患者;或未接受新辅助顺铂化疗,且不适合或拒绝接受辅助顺铂化疗,分期为pT3-pT4a或pN+的患者。
患者被随机分配至欧狄沃组(n=353)和安慰剂组(n=356),分别接受欧狄沃240 mg或者安慰剂静脉输注30分钟以上、每两周一次的治疗,直至复发或出现不可耐受的毒性,最长治疗时间为1年。符合条件的患者按1:1比例随机分配至欧狄沃组和安慰剂组,并按病理性淋巴结状态(N+ vs. N0/x [切除淋巴结数<10] vs. N0[切除淋巴结数≥10])、肿瘤细胞表达PD-L1情况(≥1% vs.<1%/不确定,由中心实验室使用PD L1 IHC 28-8 pharmDx分析确定)、以及是否使用顺铂新辅助治疗(是 vs.否)进行分层。主要疗效评价指标为研究者评估的所有随机患者和肿瘤表达PD-L1≥1%患者的DFS。DFS定义为到首次复发(局部尿路上皮、局部非尿路上皮或远处转移)或死亡的时间。其他疗效评价指标包括总生存期。FDA批准的欧狄沃剂量为每两周240 mg(30min静脉滴注)或每四周480 mg(30min静脉滴注),直至疾病复发或出现不可耐受毒性,治疗时间最长为1年。
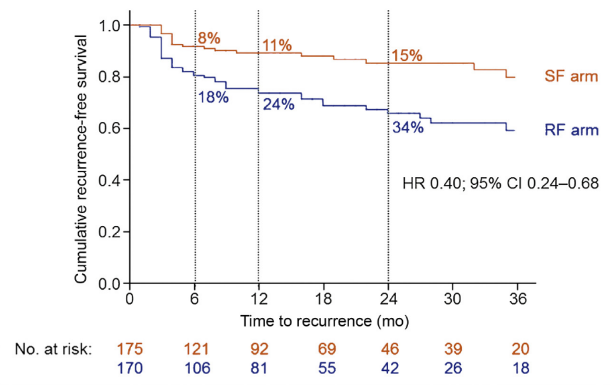
结果显示,接受欧狄沃治疗的患者中位无病生存期(DFS)是安慰剂对照组患者的近两倍(20.8个月 [95% 可信区间(CI):16.5-27.6] vs 10.8个月[95% CI: 8.3-13.9])1。与安慰剂相比,欧狄沃将疾病复发或死亡风险降低30%(风险比 [HR] 0.7, 95% CI: 0.57-0.86; P=0.0008)。在肿瘤表达PD-L1 ≥1%的患者中,欧狄沃治疗组的中位DFS未达到(95% CI:21.2-未评估;n=140),安慰剂对照组DFS为8.4个月(95% CI: 5.6-21.2; n=142),欧狄沃将疾病复发或死亡风险降低45%(HR 0.55, 95% CI: 0.39-0.77;P=0.0005)。
在安全性方面,18%的患者出现了导致停用欧狄沃的不良反应。33%的患者因为不良反应延迟了欧狄沃的使用。30%接受欧狄沃的患者出现了严重不良反应。接受欧狄沃治疗患者最常见的严重不良反应(≥2%)为尿路感染。1%的患者发生了致命的不良反应,包括肺炎(0.6%)。最常见(≥20%)不良反应为皮疹(36%)、疲劳(36%)、腹泻(30%)、瘙痒(30%)、肌肉骨骼疼痛(28%)和尿路感染(22%)。
“此次获批对于经膀胱根治性切除术或手术切除部分尿路的患者而言,是重要的里程碑。这部分患者迫切需要新的治疗选择来帮助他们降低尿路上皮癌术后复发的风险” ,CheckMate -274主要研究者、西奈山伊坎医学院Tisch肿瘤研究所泌尿生殖系统肿瘤学主任、膀胱癌卓越中心联合主任以及转化研究副主任Matthew D.Galsky教授表示: “基于CheckMate -274研究中取得的安全性和有效性研究结果,经FDA批准,纳武利尤单抗提供了一种全新治疗方式,可有效降低疾病的复发或死亡风险,并有望成为该类患者的治疗新标准” 。
使用欧狄沃的警告和注意事项:严重和致命的免疫介导的不良反应,包括肺炎、结肠炎、肝炎和肝脏毒性、内分泌疾病、皮肤不良反应、伴肾功能不全的肾炎、其他免疫介导不良反应;输液相关反应:异基因造血干细胞移植的并发症(HSCT);胚胎-胎儿毒性;当欧狄沃与沙利度胺类似物和地塞米松联用时,会增加多发性骨髓瘤患者的死亡率,因此不建议在对照临床试验之外使用。
“百时美施贵宝在免疫治疗领域的前沿探索已帮助改变了众多癌症的治疗实践。未来,我们也将持续努力,让更多创新突破惠及癌症早期患者,尤其是那些存在重大且未满足需求的患者” ,百时美施贵宝美国心血管、免疫学和肿瘤学高级副总裁兼总经理Adam Lenkowsky表示: “欧狄沃是全球首个被批准用于辅助治疗的PD-1抑制剂,尿路上皮癌是其获批用于辅助治疗的第三个癌种。这部分患者此前在预防术后疾病复发方面未有获批的标准治疗方案。伴随此次获批,我们为广大医务工作者和尿路上皮癌患者带来了新的希望” 。
CheckMate -274的研究结果还为欧狄沃于2017年2月获得FDA加速批准用于以下人群提供了确证性证据,患者人群包括:局部晚期或转移性尿路上皮癌,且接受含铂化疗期间或之后出现疾病进展;或接受含铂化疗的新辅助治疗或辅助治疗后12个月之内出现疾病进展的患者。该研究结果最终支持欧狄沃上述适应症从FDA加速批准转换为常规批准。
据悉,欧狄沃*于2014年7月获批成为全球首个PD-1抑制剂,目前已在66个国家和地区获批共11个瘤种,涵盖肺癌、头颈癌、胃癌、食管癌、肝癌、肾癌、结直肠癌、尿路上皮癌、黑色素瘤、霍奇金淋巴瘤、胸膜肿瘤,惠及超过590,000名全球患者。
参考资料:
- Opdivo Prescribing Information. Opdivo U.S. Product Information. Last updated: August 2021. Princeton, NJ: Bristol-Myers Squibb Company.
- U.S. Food & Drug Administration. Real-Time Oncology Review Pilot Program. https://www.fda.gov/about-fda/oncology-center-excellence/real-time-oncology-review-pilot-program. Accessed August 03, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#抑制剂#
31
#PD-1抑制剂#
38
#上皮癌#
40
阿库拉巨塔
57
太鼓舞人心了!
58
新的希望
0
感谢分享
43