Phytomedicine:多组学方法观察真武补气汤对慢性结肠炎的治疗作用及机制
2022-04-05 紫菀款冬 MedSci原创
采用多组学和网络药理学相结合的方法,探索真武补气汤对实验性小鼠结肠炎的全身作用及其机制。
背景:炎症性肠病(IBD)如溃疡性结肠炎(UC)可以通过药物缓解(消炎药,糖皮质激素和免疫抑制剂),但目前治疗炎症性肠病的药物存在明显的缺点,如副作用、高成本、复发、甚至恶化。从中医角度开发新的治疗策略来管理和治疗IBD是有必要的。
真武补气汤(ZWBQD)是由真武汤(ZWD)改良而来的中药配方,由茯苓、白芍、白术、姜、党参、黄连等组成,可用于治疗溃疡性结肠炎。之前的研究报道了ZWBQD减轻了右旋糖酐硫酸钠(DSS)诱导小鼠结肠炎。然而ZWBQD的生物活性成分及其分子靶点,以及治疗结肠炎作用的信号通路尚不清楚。
目的:了解ZWBQD对实验性小鼠结肠炎的全身作用及其机制。
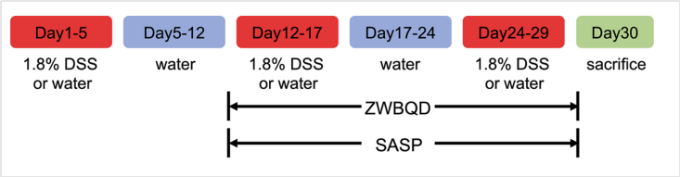
方法:将小鼠随机分为6组——对照组、DSS组、不同剂量ZWBQD组(7、14、21 g/kg/d,相当于临床用量0.71、1.42、2.13 g/kg/d)和柳氮磺胺吡啶组(SASP,50 mg/kg/d)。采用3个周期1.8% DSS诱导慢性结肠炎,试验周期为30天。
采用Luminex法测定结肠匀浆中TNF-α、IL-1β、IL-17A和IL-6的浓度。基于植物化学分析结果和网络数据库(TCMSP和TCMID数据库)构建预测靶点-信号通路数据库,收集靶点并导入到蛋白质相互作用网络中,利用STRING数据库(http://string-db.org)分析预测靶点的蛋白-蛋白相互作用,并构建靶点-信号通路数据库。
采用RNA测序、蛋白免疫印迹和肠道菌群检测,研究ZWBQD对DSS诱导的慢性大肠炎小鼠的药理作用及其机制。
结果:ZWBQD通过调节PI3K-AKT、MAPK信号通路和NF-κB信号通路,具有明显的抗炎作用,对DSS诱导的大肠炎小鼠结肠损伤有明显的保护作用。此外,ZWBQD能显著改善DSS诱导的肠道菌群失调和色氨酸分解代谢异常。
结论:该研究采用多组学和网络药理学相结合的方法,研究了ZWBQD对DSS诱导的小鼠慢性结肠炎的治疗作用及其机制。该研究发现,ZWBQD对小鼠慢性结肠炎具有明显的抗炎和保护作用,并鉴定了ZWBQD的主要植物化学成分。
ZWBQD作用的药理机制与抑制结肠组织中的“PI3K-AKT信号通路”、“MAPK信号通路”和“NF-κB信号通路”以及调节肠道微生物代谢有关。此外,该研究中描述的多组学和网络药理学综合方法可以应用于未来的研究中,评价补充和替代药物的治疗效果和药理机制,如中医药作为治疗炎症性肠病的新疗法。
文献来源:
Zhai L, Peng J, Zhuang M, et al. Therapeutic effects and mechanisms of Zhen-Wu-Bu-Qi Decoction on dextran sulfate sodium-induced chronic colitis in mice assessed by multi-omics approaches [published online ahead of print, 2022 Feb 25]. Phytomedicine. 2022;99:154001. doi:10.1016/j.phymed.2022.154001
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#CIN#
33
#DIC#
40
学习,打卡
73
#Medicine#
41
#Med#
40
学习了,谢谢分享
55