Cell:DNA损伤揭示抗癌新疗法
2015-09-06 佚名 生物谷
大自然中每一个有机体都会不惜代价保护自身的DNA,但细胞如何精确区分自身DNA的损伤还是入侵病毒外源DNA的损伤依然是个谜底,近日刊登在国际杂志Cell上的一篇研究论文中,来自索尔克研究所的研究人员通过研究揭示了细胞反应系统精确区分上述两种威胁的机制,相关研究或可帮助开发新型的癌症选择性病毒疗法,同样也可以帮助理解为何老化和某些疾病似乎总在为病毒感染敞开着大门。研究者Clodagh O'Shea教
大自然中每一个有机体都会不惜代价保护自身的DNA,但细胞如何精确区分自身DNA的损伤还是入侵病毒外源DNA的损伤依然是个谜底,近日刊登在国际杂志Cell上的一篇研究论文中,来自索尔克研究所的研究人员通过研究揭示了细胞反应系统精确区分上述两种威胁的机制,相关研究或可帮助开发新型的癌症选择性病毒疗法,同样也可以帮助理解为何老化和某些疾病似乎总在为病毒感染敞开着大门。
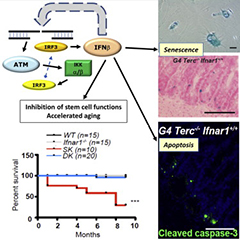
研究者Clodagh O'Shea教授说道,本文研究阐明了一种基本的机制,即机体如何区分细胞和病毒基因组的DNA断裂来诱发不同的保护宿主的免疫反应,该研究或可帮助解释为何特定的状况,比如老化、癌症化疗以及炎症使我们机体对病毒感染变得更加敏感。
许多因子都会引发DNA断裂,研究者在文章中阐明了名为MRN复合体的一系列蛋白如何检测DNA和病毒的破裂,并且通过组蛋白来放大这种效应;MRN复合体蛋白会开启一种多米诺骨牌效应,激活染色体周围的组蛋白,最终引发一种广泛的效应来帮助机体细胞修复DNA。
一般来讲,常见的DNA病毒进入宿主细胞核后会开启复制自身DNA的基因的表达,而宿主细胞则会检测到这种未授权的复制,同时MRN复合体就会在不诱发杀细胞的广泛反应的前体下选择性地中和病毒的DNA,MRN对病毒的反应会在局部停留并且会仅仅选择性地抑制病毒;如果入侵的病毒会引发类似强烈的反应,那么细胞将会频繁地暂停生长。
文章中,研究者开发了新型病毒,其可以在正常细胞中被破坏,但可以在癌细胞中进行特异性复制,并不像正常细胞,癌细胞几乎总是包含高水平的DNA损伤,在癌细胞中,MRN或许会针对DNA破裂做出反应,但工程化的病毒或许就可以逃脱监视。癌细胞总是存在较高的突变率,而且在早期阶段会存在基因组的不稳定性,因此我们可以想象一下构建一种病毒来破坏早期机体损伤以及作为预防措施是多么困难的事情。
原文出处:
Govind A. Shah, Clodagh C. O’Shea.et al.Viral and Cellular Genomes Activate Distinct DNA Damage Responses.Cell.2015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#CEL#
56
#抗癌新疗法#
64
#Cell#
53
期待进一步的研究
143
期待进一步的研究
80
期待进一步的研究
121
期待进一步的研究
52
期待进一步的研究
153
期待进一步的研究
144
期待进一步的研究
83