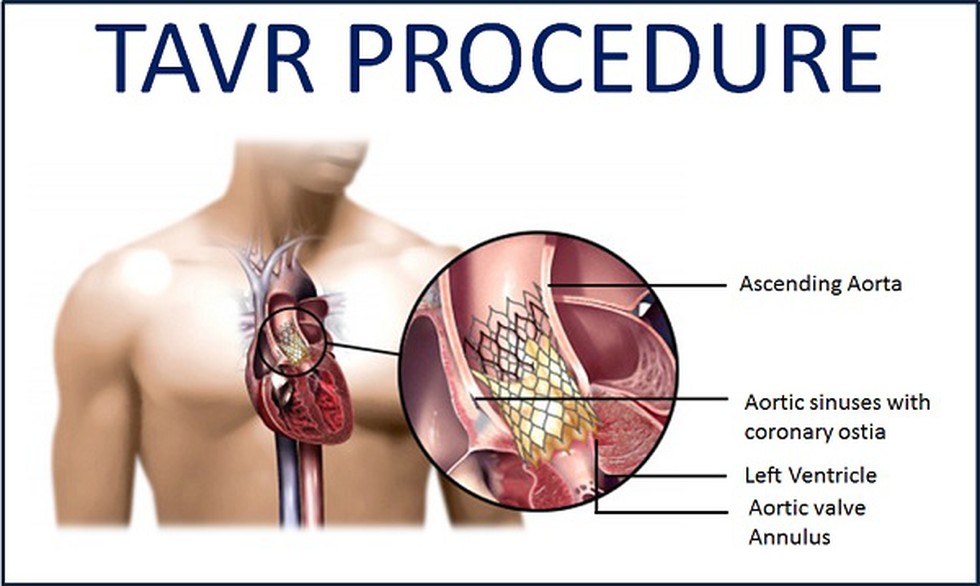
主动脉瓣置换术(AVR)是有症状重度主动脉瓣狭窄(AS)的主要治疗手段。经导管主动脉瓣植入术(TAVI)也称经导管主动脉瓣置换术(TAVR),其替代外科主动脉瓣置换术(SAVR)的作用正在不断演变。
在经皮主动脉瓣置换术或TAVI中,置换的瓣膜经腹股沟处的股动脉导管,向上达到升主动脉。这一技术取代了更具创伤性的开胸手术。两者的术后生存率相持平,但是经导管术的中风风险更高。
2018年发表在国际心血管权威杂志JACC上的研究评估低流量低压差主动脉瓣狭窄(LFLG-AS)患者TAVR后的临床预后及左室射血分数(LVEF)的变化。结果显示,TAVR在LFLG-AS患者中的围手术期疗效较好,但同时副作用的发生率也更高。
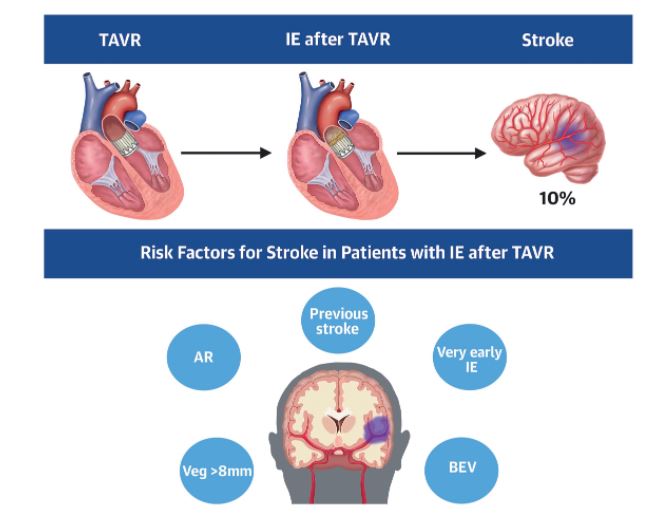
其中,中风是感染性心内膜炎(IE)最常见和最有可能致残的并发症之一。然而,关于TAVR后IE并发中风的数据很少。为此,来自加拿大、德国、法国等多中心的心脏病学专家研究了TAVR术后后并发卒中的风险,结果发表在最新的JACC上。
研究人员分析了TAVR术后感染性心内膜炎国际登记处的数据(包括11个国家59个中心的569名TAVR术后发生明确IE的患者)。根据IE入院期间发生卒中的情况,将患者分为两组(卒中[S-IE]与无卒中[NS-IE])。目的是确定TAVR术后明确的IE患者在索引IE住院期间并发卒中的发生率、危险因素、临床特征、管理和结果。
结果共有57名(10%)患者在IE住院期间发生了中风,两组之间致病微生物比较没有差异。S-IE患者表现出较高的急性肾衰竭、全身性栓塞和持续菌血症的比率(P<0.05)。同时,IE前的卒中、TAVR后残留的主动脉瓣反流≥中度、球囊扩张的瓣膜、TAVR后30天内的IE、瓣膜大小>8mm与IE患者住院期间的卒中风险较高有关(P<0.05)。
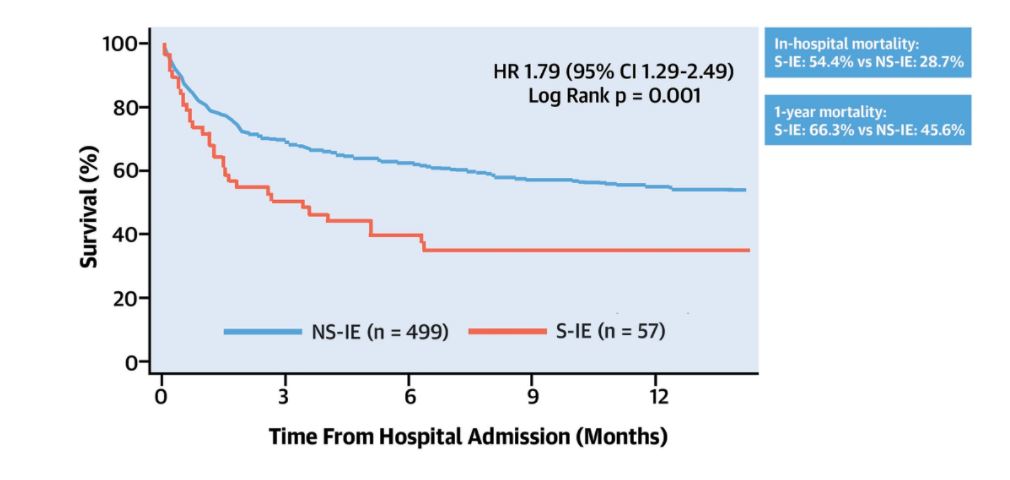
TAVR术后两组间患者随时间变化的生存时间差异
没有危险因素的患者中风率为3.1%,如果存在>3个危险因素,中风率会增加到60%。S-IE患者的院内死亡率(54.4% vs. 28.7%;p < 0.001)和1年后的总死亡率(66.3% vs. 45.6%;p < 0.001)更高。手术治疗与S-IE患者的预后改善无关(院内死亡率:手术治疗的46.2% vs. 无手术治疗的58.1%;P = 0.47)。
由此可见,10名TAVR术后的IE患者中,有1人发生了中风。有中风病史、TAVR和IE之间的时间短、瓣膜大小、瓣膜假体类型和残留的主动脉反流决定了风险增加。此外,中风的发生与院内和1年死亡率的增加有关,手术治疗未能改善临床结果。
综上,经导管主动脉瓣置换术后并发卒中的风险不容忽视!
参考文献:
Del Val D, et al. Stroke Complicating Infective Endocarditis After Transcatheter Aortic Valve Replacement. J Am Coll Cardiol. 2021 May 11;77(18):2276-2287. doi: 10.1016/j.jacc.2021.03.233.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#置换#
39
#JACC#
47
#并发#
42
#ACC#
34
#主动脉瓣#
32
#主动脉瓣置换术#
45
#主动脉#
36
#经导管#
34
#经导管主动脉瓣置换#
38
#置换术#
30