J Am Coll Cardiol:利伐沙班致命性或不可逆性出血和缺血性事件知多少
2018-08-29 佚名 环球医学网
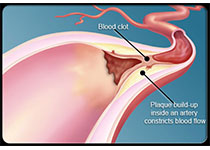
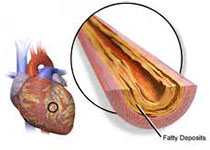
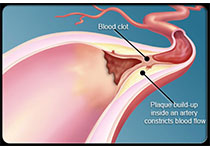
发表在《J Am Coll Cardiol》的一项研究,调查了急性冠状动脉综合征患者(ACS)中利伐沙班的致命性或不可逆性出血和缺血性事件。
目的:鉴于这些事件具有相似的临床影响,因此有效性和安全性的比较仅限于致命性或不可逆性缺血性和不良或严重有害事件,这是评估净临床结局和总体风险获益的一种方法。
方法:在ATLAS ACS 2-TIMI 51试验(降低心血管事件的抗Xa治疗以及ACS-心肌梗死溶栓治疗的标准治疗)中,利伐沙班用于阿司匹林+氯吡格雷或噻氯匹定(氯吡格雷/噻氯匹定)或仅阿司匹林治疗的ACS患者事件的二级预防,该试验将致命性和不可逆性有效性事件定义为非出血性心血管死亡、心肌梗死和缺血性卒中,将致命性或不可逆性安全性事件定义为致命性和颅内出血,并将有效性事件和安全性事件进行了比较。
结果:在每10000患者年的暴露中,阿司匹林+氯吡格雷/噻氯匹定治疗的患者,使用口服利伐沙班2.5mg每天两次,与致命性或不可逆性缺血性事件减少115(95% CI,18~212)(安慰剂vs治疗:663 vs 548)和额外致命性或不可逆性严重有害事件增加10(95% CI,-11~32)(33 vs 23)相关。一起考虑时,与安慰剂相比,每10000患者年的利伐沙班暴露,可预防105例(95% CI,6~204)致命性或不可逆性事件,对于预防造成的每例致命性或不可逆性严重有害事件,可预防11(10/115)例致命性或不可逆性缺血性事件。如果仅将非大出血心血管死亡纳入为致命性或不可逆性事件,那么口服利伐沙班2.5mg每天两次的患者,每10000患者年的暴露,可预防95例事件。
结论:致命性或不可逆性缺血和出血是临床显着的事件,二者可以用于比较,从而评估治疗带来的净临床结局。阿司匹林+氯吡格雷治疗的患者每天两次口服2.5mg剂量的利伐沙班,与致命性或不可逆性事件的净减少相关。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#缺血性#
30
#Cardiol#
38
#Coll#
41
好文章,谢谢分享!
55
好文章,谢谢分享!
68
好文章,谢谢分享!
60
好文章,谢谢分享!
1
好文章,谢谢分享!
65
好文章,谢谢分享!
20
好文章,谢谢分享!
25