8种常见腹痛的特点
2016-07-23 北京大学人民医院腔镜外科 钟朝辉 人民网
1.一阵一阵的绞痛推测病因:肠梗阻严重后果:肠穿孔、肠坏死、休克肠梗阻引起的肚子疼主要是一阵儿一阵儿的绞痛,整个肚子还会打了气儿一样的胀,有的患者还会呕吐,不放“噗噗”、也不“嗯嗯”,整个肠子就像被堵住了一样。如果变成了持续性的绞痛,并且一波比一波疼,就有可能转成了更严重的绞窄性肠梗阻。造成肠梗阻的病因比较多,常见的有便秘、炎症、机械性的梗阻(肠外压迫、肠套叠、肠扭转、粪块异物梗阻)、还有肠道肿瘤
推测病因:肠梗阻
严重后果:肠穿孔、肠坏死、休克
肠梗阻引起的肚子疼主要是一阵儿一阵儿的绞痛,整个肚子还会打了气儿一样的胀,有的患者还会呕吐,不放“噗噗”、也不“嗯嗯”,整个肠子就像被堵住了一样。如果变成了持续性的绞痛,并且一波比一波疼,就有可能转成了更严重的绞窄性肠梗阻。造成肠梗阻的病因比较多,常见的有便秘、炎症、机械性的梗阻(肠外压迫、肠套叠、肠扭转、粪块异物梗阻)、还有肠道肿瘤等。如果不及时治疗,会造成肠道穿孔、肠坏死、感染性休克,甚至死亡。
2.右边小肚子疼,还乱窜
推测病因:阑尾炎
严重后果:阑尾穿孔、脓肿
阑尾炎,一般疼着疼着还会换地方。最典型的是从肚子上边开始疼,逐渐往下挪到了肚脐周围,最后转移到右边小肚子,也就是右下腹,并且在这儿安营扎寨使劲疼。它的特点是,疼痛一旦转移到右下腹,之前那些疼过的部位就不疼了。而且多数患者都会发低烧,即使是化脓性阑尾炎也不会超过38℃,如果是高热,很有可能是发生了阑尾炎穿孔,甚至是腹膜炎。
阑尾炎如果不及时治疗会造成穿孔、阑尾周围脓肿等并发症。
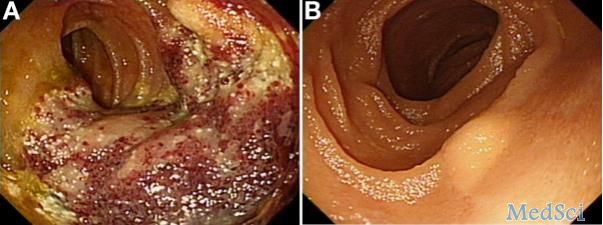
3.大吃大喝后肚子疼
推测病因:胰腺炎
严重后果:脓肿,感染,死亡
胰腺炎引起的肚子疼常常出现在吃过大量油腻腻的食物后,或者大量饮酒后,疼痛一般位于肚子的中上部,有时候会向腰部、背部嗖嗖放射着疼。疼痛程度因人而异,病情轻的就是钝痛,病情重的就会有持续性的绞痛。轻症的胰腺炎没有什么并发症,重症的胰腺炎会造成胰腺脓肿,还可能造成腹腔的感染、多器官的衰竭。需要注意的是,重症胰腺炎的死亡率很高,如果不早期控制住,死亡率甚至可以达到40% ——50%。
4.肚子右边刀割样的绞痛
推测病因:胆囊炎
严重后果:穿孔
急性胆囊炎引起的疼痛,位置是在肚子右边,患者会感觉像刀割一样绞着疼(想象一把尖刀在肚子里旋转跳跃…),一阵一阵发作,发作时也没有预兆,剧烈的疼痛经常打得患者措手不及,可能还会伴随着恶心呕吐和发热,一般热度在38.5度以下,有的患者还会有右肩膀的放射疼。胆囊炎不及时治疗可能会造成胆囊穿孔和胆囊周围脓肿,肝脓肿,但这种严重的后果比较少见。
5.育龄女性整个肚子都疼
推测病因:宫外孕
严重后果:大出血
宫外孕引起的疼痛是整个肚子都在疼,宫外孕破裂出血前,患者会感觉特别疼,破裂出血后,疼痛反而会感觉轻了一点。宫外孕最常见的并发症是腹腔内的出血。随着医疗条件的改善,宫外孕的死亡率已经没有那么高了,但是一旦发作,病情通常比较凶险。
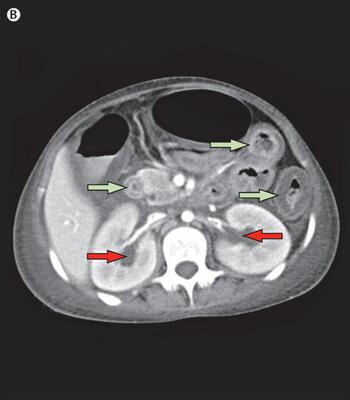
6.腰腹部疼,下体也疼
推测病因:泌尿结石
严重后果:休克
泌尿系统结石最典型的症状就是肾绞痛和血尿。如果一边腰腹部突然超级疼,还沿着输尿管嗖嗖的向下半身(睾丸、阴囊、大阴唇)放射着疼,就非常可能是肾绞痛。肾绞痛主要是由于肾脏内的结石掉进了输尿管,并且顺着输尿管向下蠕动排出时引起的。它疼起来特别突然,特别剧烈,这种绞痛可以持续几分钟到几十分钟,有的人还会疼几个小时。疼痛发作时,患者还可能会恶心呕吐、大汗淋漓、面色苍白、辗转不安,严重的还会休克。
7.肚子上有个包,剧痛
推测病因:嵌顿疝
严重后果:肠壁缺血坏死
疝气就是人体内某个零件离开自己的位置,钻到了别的地方。发生疝气的部位,通常会鼓个包,所以很容易发现。疝气本来不疼,有时会有往下坠、酸胀的感觉,但如果发生了嵌顿,患者就会剧烈疼痛。所谓嵌顿疝,就是它钻到别人的地盘结果被卡住,回不去了,这种疼痛刚开始是一阵一阵的,随后就会疼得停不下来。除了剧烈的疼痛,患者还会出现呕吐,停止排气、停止排便等肠梗阻的症状。如果发生嵌顿的是肠管,它被持续卡着,肠子就会因为没有血液供应而坏死,后果是很严重的。
8.心脑血管病人突然肚子绞痛
严重后果:肠坏死
肠系膜血管栓塞引起的腹痛,是非常剧烈的持续性的疼痛,疼痛部位常在上腹部,肚脐周围或者右上腹,患者常常还会恶心、呕吐、腹泻。一般情况下是毫无预兆,突然就疼起来了,解痉类药物很难缓解这种疼痛。这个病如果不及时处理,会引起大面积的肠坏死,所以还是很凶险的。有心脑血管病的患者一定要多加小心。
上面是一些腹痛基本特点的总结,但是临床上不能生搬硬套,需要根据患者临床表现和相关辅助检查综合判别。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











文章不错,值得拜读
65
文章不错,值得拜读
60
讲的细致
57
#腹痛#
30
讲的很全面
62