STM:新策略让乳腺癌告别“骨转移”
2016-05-28 佚名 生物探索
5月25日,杜克癌症研究所的科学家在Science Translational Medicine揭示了乳腺癌骨转移的另一个关键分子,并提出阻止乳腺癌骨转移的策略。 去年,科学家在《Nature》上揭示了乳腺癌细胞分泌蛋白lysyl oxidase(LOX)经血液循环到达骨骼,产生溶骨作用,从而帮助乳腺癌细胞在骨骼中转移。5月25日,杜克癌症研究所的科学家在 Science Translati
5月25日,杜克癌症研究所的科学家在Science Translational Medicine揭示了乳腺癌骨转移的另一个关键分子,并提出阻止乳腺癌骨转移的策略。
去年,科学家在《Nature》上揭示了乳腺癌细胞分泌蛋白lysyl oxidase(LOX)经血液循环到达骨骼,产生溶骨作用,从而帮助乳腺癌细胞在骨骼中转移。5月25日,杜克癌症研究所的科学家在 Science Translational Medicine 揭示了乳腺癌骨转移的另一个关键分子,并提出阻止乳腺癌骨转移的策略。
通过对小鼠的多年试验,科学家找到了一种策略既能预防乳腺癌细胞进入骨髓又能将其“驱赶”至血液中,使其更容易被摧毁。研究人员认为如果该研究结果能在其他动物和人体试验中复制,那么将给乳腺癌的治疗带来新的途径。
本研究资深作者,杜克癌症研究所血液系统恶性肿瘤及细胞疗法助理教授Dorothy A. Sipkins医学博士表示,“临床研究发现,乳腺癌可在早期被发现并治疗,但一个无疾病症状的患者,在10年或15年后,也可能出现疾病复发,且最常见的肿瘤转移部位是骨骼。”
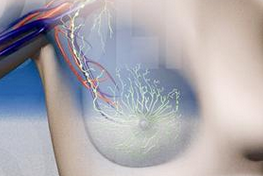
在该研究中,研究人员描述了激素受体阳性乳腺癌细胞如何在血液和组织中“漫步”,他们发现这些癌细胞在寻找骨髓中包含E-selectin分子的特殊血管,并借助其表面特殊分子与E-selectin分子的结合进入骨骼中的海绵组织,且通常情况下这些细胞可潜伏多年。
为告别乳腺癌骨转移提供策略
根据美国临床肿瘤学会,激素受体阳性乳腺癌是最常见的乳腺癌类型,借助人体雌激素或孕激素来生长。本文资深作者Sipkins医学博士说,“在人类患者中,这些休眠细胞可在后期复苏并造成转移癌复发,且无法治愈。人类乳腺癌骨髓活检显示,即使在非常早期的癌症阶段,”漫游“的癌细胞(或微转移)就已经拥有独特的方式离开乳腺进入骨髓。”
研究人员表示,“如今我们知道了这些癌细胞如何进入骨骼,同时我们还确定了其锚定骨骼的重要机制。在该研究中,我们通过小鼠试验提供了新的策略——在休眠细胞扎根及复发前在分子水平上对其进行干预。”
策略之一是寻找一种方法来抑制E-selectin分子,这有助于限制癌细胞进入骨骼以及复发的能力。在该研究中,研究人员选用的E-selectin抑制剂为GMI-1271,该分子目前正用于人体临床试验中,研究人员发现该化合物能成功阻止乳腺癌细胞进入小鼠的骨髓中。
由于乳腺癌细胞扩散至骨骼可发生在疾病被诊断前的早期阶段里,因此研究人员还研究了一种策略将乳腺癌细胞从骨骼中“踢开”,使其返回到血液中。为了实现该目的,研究人员给小鼠注射plerixafor,plerixafor是一种用于人骨骼中的药剂,目的是将干细胞推入血液中。研究人员发现,plerixafor能使处于休眠状态的乳腺癌细胞从骨组织中流出并进入血液中。研究人员推测,将这些休眠的癌细胞从骨骼“驱赶”至血液,可增加其被免疫系统(化疗或激素)杀死的概率。
Sipkins说,“我们希望通过了解乳腺癌细胞如何在体内迁徙以及它们的生命周期如何,从而找出更有效的治疗方法,我们希望在老鼠身上做更多的研究,为人类研究打更好的基础。”
原始出处:
Price TT, Burness ML, Sivan A, Warner MJ, Cheng R, Lee CH, Olivere L, Comatas K, Magnani J, Kim Lyerly H, Cheng Q, McCall CM, Sipkins DA.
Sci Transl Med. 2016 May 25;8(340):340ra73. doi: 10.1126/scitranslmed.aad4059.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















拜读,好文
49
#STM#
30
关注能否在临床中开展研究!
112
关注能否在临床中开展研究!
122
#新策略#
34
期待下一步研究
166
期待下一步研究
132
期待进一步研究
81
希望早日实现临床应用
79
希望早日实现临床应用
98