JACC:PCI术后心肌梗死面积可预测死亡和心衰风险
2016-04-05 崔倩 译 MedSci原创
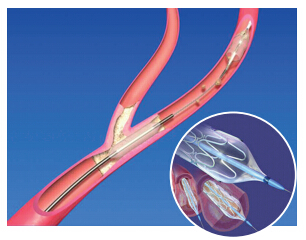
ST段抬高心肌梗死(STEMI)患者再灌注可减少梗死面积和提高生存率。然而,在当代梗死面积和预后的直观联系一直没有令人信服地被证明。本研究旨在确定在STEMI患者中早期经皮冠状动脉介入治疗(PCI)评估梗死面积和随后的心脏衰竭全因死亡率,再梗死,住院之间的关系的强度。研究人员从10个随机急诊PCI试验(共2632例患者)进行了汇集患者水平分析,其梗死面积在随机分配后1个月内通过心脏磁共振(CMR)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#JACC#
30
#PCI术#
31
#ACC#
30
#心衰风险#
25
#PCI术后#
26
学习了,很好
147
介入治疗的应用,需要临床进一步观察。
130