PLoS One:低睾丸素水平男性中,睾丸素治疗和恶性前列腺癌风险研究
2018-07-05 AlexYang MedSci原创
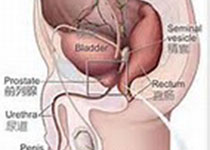
低睾丸素男性中的睾丸素治疗是非常常见的,并且尽管治疗周期短,该治疗方法还是使得人们对前列腺癌(CaP)风险的增加感到担忧。最近,有研究人员调查了持续适中睾丸素治疗与恶性CaP发生之间的关系。研究包括了2002年到2011年睾丸素水平低的患者,并且进行了前列腺特异性抗原(PSA)测试;排除了那些进行睾丸素治疗、前列腺或者乳腺癌、高PSA或者前列腺活检的患者。组织学确定的发生的恶性前列腺癌或者任何前列
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#癌风险#
26
#前列腺癌风险#
27
#风险研究#
36
#恶性前列腺癌#
30
#Plos one#
27
#睾丸#
24
#睾丸素#
32