AHA/ASA发布新版未破裂颅内动脉瘤患者管理指南
2015-06-20 cath、大鹏 编译 医学论坛网
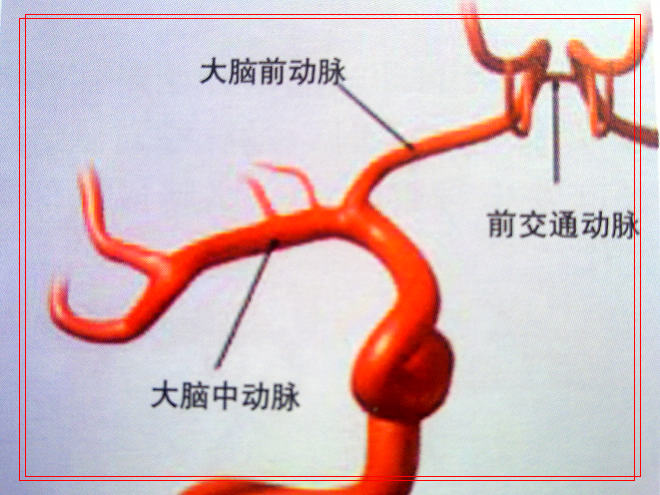
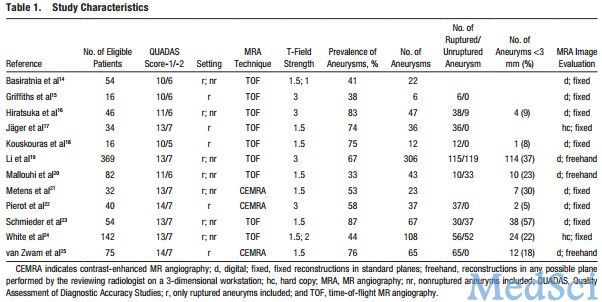
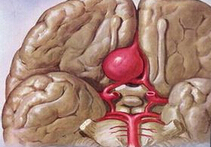
美国心脏学会/美国卒中学会(AHA/ASA)6月18日在《卒中》(STROKE)杂志发表了《未破裂颅内动脉瘤患者管理指南》(以下简称指南)。指南编写组系统回顾了1977年1月至2014年6月的文献,在基于证据情况下,对未破裂颅内动脉瘤(UIA)患者的自然病史、流行病学、危险因素、筛查诊断、影像学以及外科和血管内治疗的转归等方面提出了一系列建议。详细内容如下:一、动脉瘤进展、增长和破裂的危险因素
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#ASA#
29
#管理指南#
32
总结也很到位
81
希望能有用吧
109
这篇文章写得很好
149
收藏
97
学习指南
152
#AHA#
33
#患者管理#
0
!
82