Cancer Gene Ther:去势抵抗性前列腺癌细胞中的基因疗法研究
2019-02-14 AlexYang MedSci原创
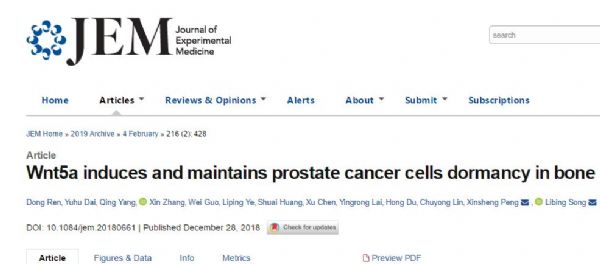
前列腺癌是全球范围内男性的第二大癌症。晚期阶段的前列腺癌患者通常通过雄激素阻断疗法(ADT)来治疗。然而,随着疾病的恶化,常常会发展成为不可治愈的去势抵抗性前列腺癌(CRPC)。JC型多瘤病毒(JCPyV)是一种人类DNA病毒。它的类病毒颗粒(VLPs)展现出了与原生病毒相似的趋向性,并且具有将外源基因转化进靶细胞进行表达的能力。研究人员在前列腺细胞中检测到了JCPyV;因此,前列腺癌细胞可能对J
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Gene#
33
#抗性#
29
#癌细胞#
39
#去势抵抗性前列腺癌#
0
#前列腺癌细胞#
38