Neurology:肾功能受损患者导致中风风险增加,这种亚型尤其要注意!
2022-05-03 MedSci原创 MedSci原创
肾功能损害导致了特定卒中亚型的不同分布和临床效果,在心栓性卒中和小血管闭塞中尤为明显。
慢性肾脏病是一个世界性的公共卫生问题,被认为是中风的既定危险因素。目前仍不清楚它的分布和临床影响在肾功能受损患者的缺血性卒中亚型中是否一致。为此,来自日本福冈医院研究了肾功能损害是否与每种卒中亚型与缺血性卒中总体的比例有关,以及与每种卒中亚型后的功能结果有关,结果发表在Neurology杂志上。
研究参与者为2016年10月至2019年12月期间日本卒中数据库(一个基于医院的多中心卒中登记数据库)登记的10392名急性卒中成年患者,其基线血清肌酐水平或滴定式蛋白尿结果可获得。
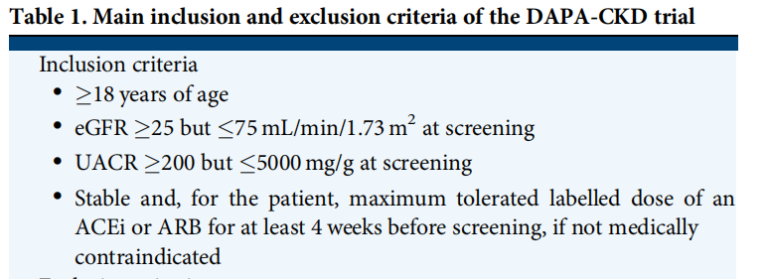
所有的缺血性中风都是根据急性中风治疗中的Org 10172试验标准进行分类。不利的功能结果被定义为出院时mRS评分3-6分。混合效应逻辑回归用于确定结果与估计肾小球滤过率(eGFR)、eGFR分层(<45,45-59,≥60 mL/min/1.73 m2)或经协变量调整后的滴速蛋白尿≥1之间的关系。
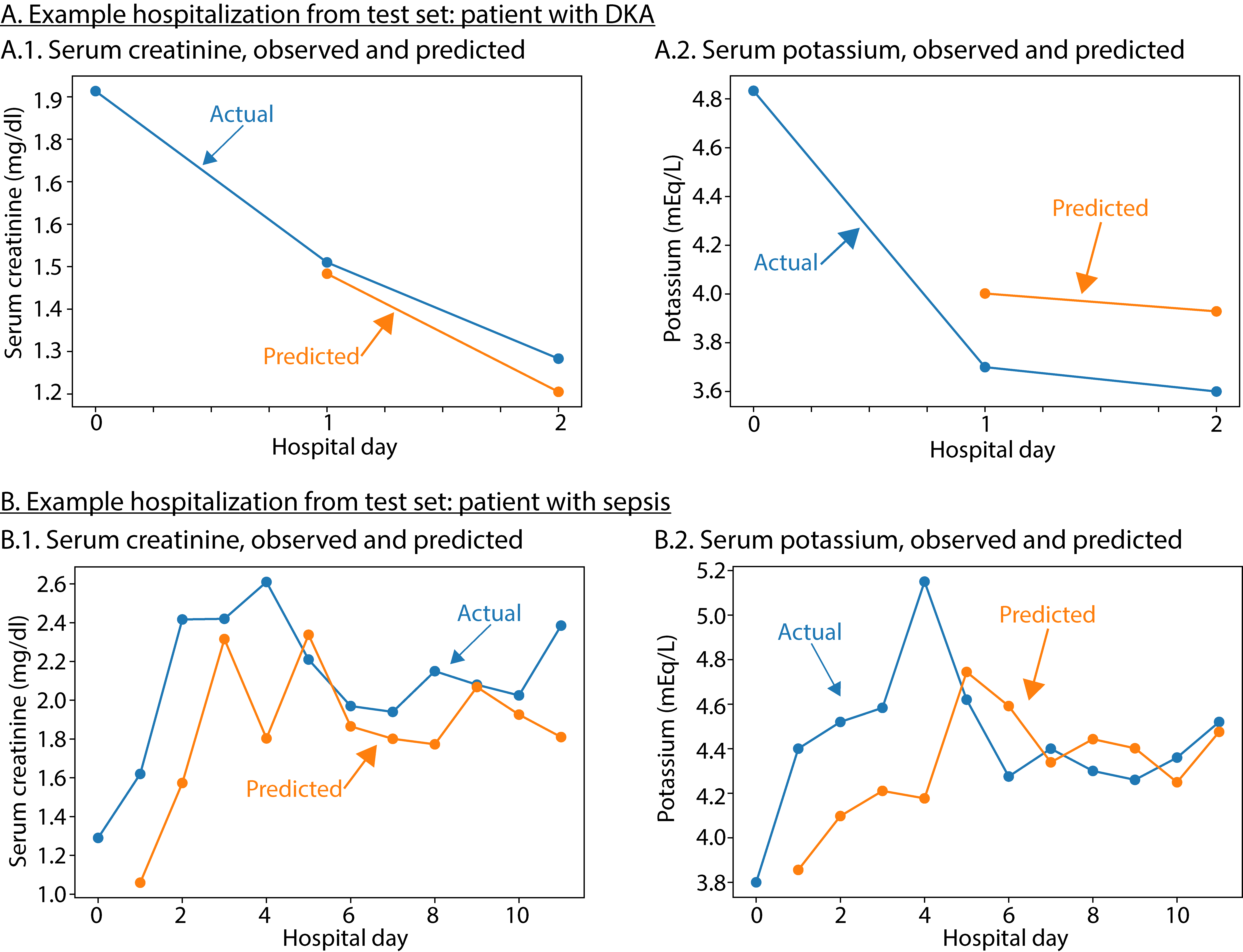
结果显示,总体而言,2419名(23%)患者的eGFR为45-59 mL/min/1.73 m2,1976名(19%)患者的eGFR<45 mL/min/1.73 m2,包括185名(1.8%)接受血液透析的患者。eGFR 45-59和eGFR<45 mL/min/1.73 m2分别与心源性脑梗风险增加21%和55%(OR=分别为1.21[95% CI,1.05-1.39]和1.55[1.34-1.79])和较低的小血管闭塞风险降低21%和32%(OR=0.79[0.69-0.90]和0.68[0.59-0.79])有关。
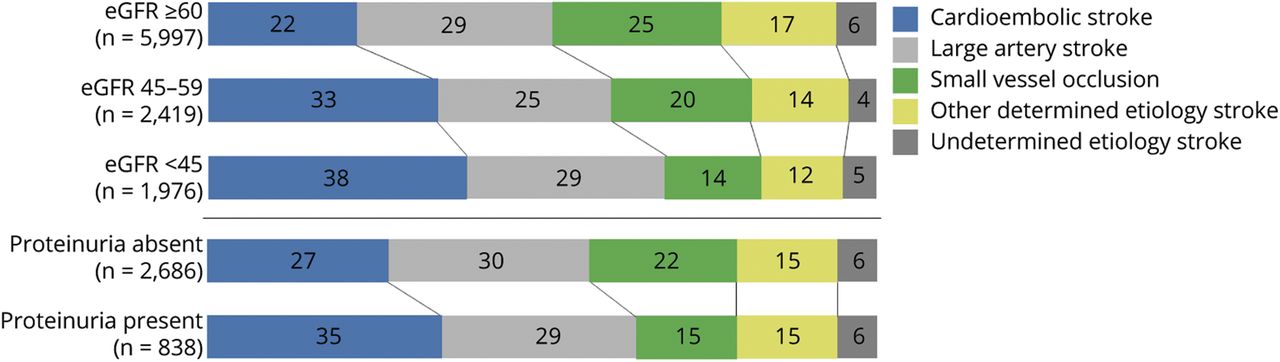
在使用eGFR下降作为连续值的分析中,证明与这2种亚型的比例有类似的关联。eGFR<45 mL/min/1.73 m2和蛋白尿都与心源性脑梗(OR=1.30[95% CI,1.01-1.69]和3.18[2.03-4.98])和小血管闭塞(OR=1.44[1.01-2.07]和2.08[1.08-3.98])患者不利的功能结局有关。
综上,肾功能损害导致了特定卒中亚型的不同分布和临床效果,在心栓性卒中和小血管闭塞中尤为明显。
参考文献:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#肾功能#
42
#中风风险#
61
#Neurol#
30
#期刊论坛#嗯
69
#期刊论坛#
76