Heart:手术和经导管主动脉瓣置换术后感染性心内膜炎的风险
2022-01-29 MedSci原创 MedSci原创
IE是接受SAVR和TAVI治疗患者罕见的并发症。在该研究人群中,SAVR后IE的发生率高于TAVI。
感染性心内膜炎(IE)是人工瓣膜置换术后一种危及患者生命的并发症,每年每1000名患者中有3-10人受IE的影响。在过去15年中,经导管主动脉瓣植入术(TAVI)彻底改变了主动脉瓣狭窄的治疗方法,导致使用人工瓣膜的患者数量增加。据报道,人工瓣膜患者的IE发病率是普通人群的100多倍,在频繁住院和有创手术治疗的老年患者中,这种风险可能更高。

近日,心脏病领域权威杂志Heart上发表了一篇研究文章,研究人员旨在明确经外科主动脉瓣置换术(SAVR)和经导管主动脉瓣植入术(TAVI)的患者感染性心内膜炎(IE)的发病率和危险因素。

研究人员从NICOR数据库中确定了2007年至2016年期间在英格兰首次接受SAVR或TAVI的所有患者,并通过与NHS医院事件统计数据库进行链接,确定了初步诊断为IE的入院患者。研究人员获得了NHS研究伦理委员会的批准。
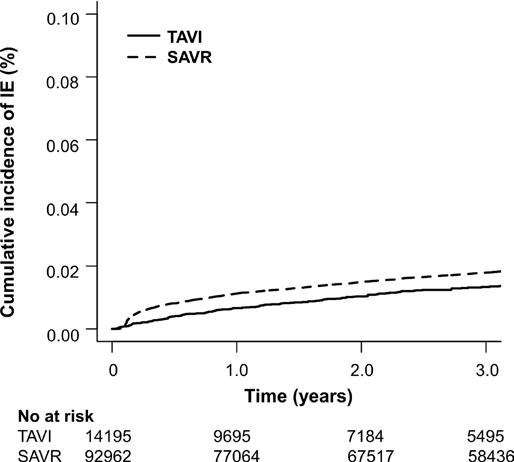
该研究纳入的91962名接受SAVR的患者中有2057人在中位随访的53.9个月内发展为IE,总发病率为每1000人每年4.81人[95%CI为4.61至5.03]。相应地,接受TAVI治疗的14195名患者中有140人在中位随访24.5个月内发展为IE,其总发病率为每1000人每年3.57[95%CI3.00至4.21]。SAVR后60个月IE的累积发生率高于TAVI(2.4%[95%CI为2.3至2.5] vs 1.5%[95%CI为1.3至1.8],HR为1.60,p<0.001)。在整个队列中,经过多变量调整后,SAVR仍然是IE的独立预测因子。IE的危险因素包括年龄较小、男性、心房颤动和透析。
由此可见,IE是接受SAVR和TAVI治疗患者罕见的并发症。在该研究人群中,SAVR后IE的发生率高于TAVI。
原始出处:
Thomas J Cahill.et al.Risk of infective endocarditis after surgical and transcatheter aortic valve replacement.heart.2022.https://heart.bmj.com/content/early/2022/01/20/heartjnl-2021-320080
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#置换#
50
TAVI的手术适应症可逐渐扩大
0
#内膜#
46
#感染性#
42
#主动脉瓣#
39
#心内膜炎#
43
#ART#
41
#主动脉瓣置换术#
54
#主动脉#
39
#经导管#
51