Infection: COVID -19阳性患者的相关凝血因子和多种止血标志物都会存在异常
2022-10-14 xuyihan MedSci原创
COVID-19一般指新型冠状病毒肺炎。 新型冠状病毒肺炎(Corona Virus Disease 2019,COVID-19),简称“新冠肺炎”,世界卫生组织命名为“2019冠状病毒病”。
凝血功能障碍仍然是一种严重的、尚未被充分理解的COVID -19患者的并发症。它的形式和严重程度可以决定患者的治疗方案及其结果。虽然D-二聚体已被证明可以反映 COVID-19 患者的严重程度和预后,但凝血酶原时间 (PT)、国际标准化比值 (INR)、部分促凝血酶原激酶时间 (APTT) 和纤维蛋白原的作用尚不明确。免疫血栓相关 COVID-19 感染被认为与 COVID 相关凝血病 (CAC) 的发病机制相关。由于内皮细胞损伤是COVID-19发病机制中的一个恒定特征,血管性血友病因子 (VWF) 和因子 VIII (FVIII) 过量、释放和升高程度可能是一个很好的诊断和预后标志物疾病。本项研究旨在评估患有COVID-19的患者相关凝血病和多种止血标志物。此外,评估凝血急性期反应物及其对结果的影响。

该研究包括106名COVID-19患者和 51名对照患者。所有患者的鼻咽拭子检测COVID-19 感染均呈阳性。除了基线数据和放射学检查结果外,凝血曲线还特别关注纤维蛋白原、D-二聚体、因子 VIII、血管性血友病因子 (VWF)、蛋白 C、蛋白 S、抗凝血酶 III (ATIII) 和狼疮抗凝剂 (LA )-1 和 2的水平差异。
研究结果显示COVID-19阳性患者的VWF、D-二聚体和 LA1和 LA2显着高于对照组。在严重COVID-19症状患者组中检测到显着更高的D-二聚体 FVIII、VWF 和 LA1-2。ATIII ,而且有很高的诊断准确性。同时,研究人员发现血栓事件患者的国际随机比率 (INR) 和 VWF 显着升高。
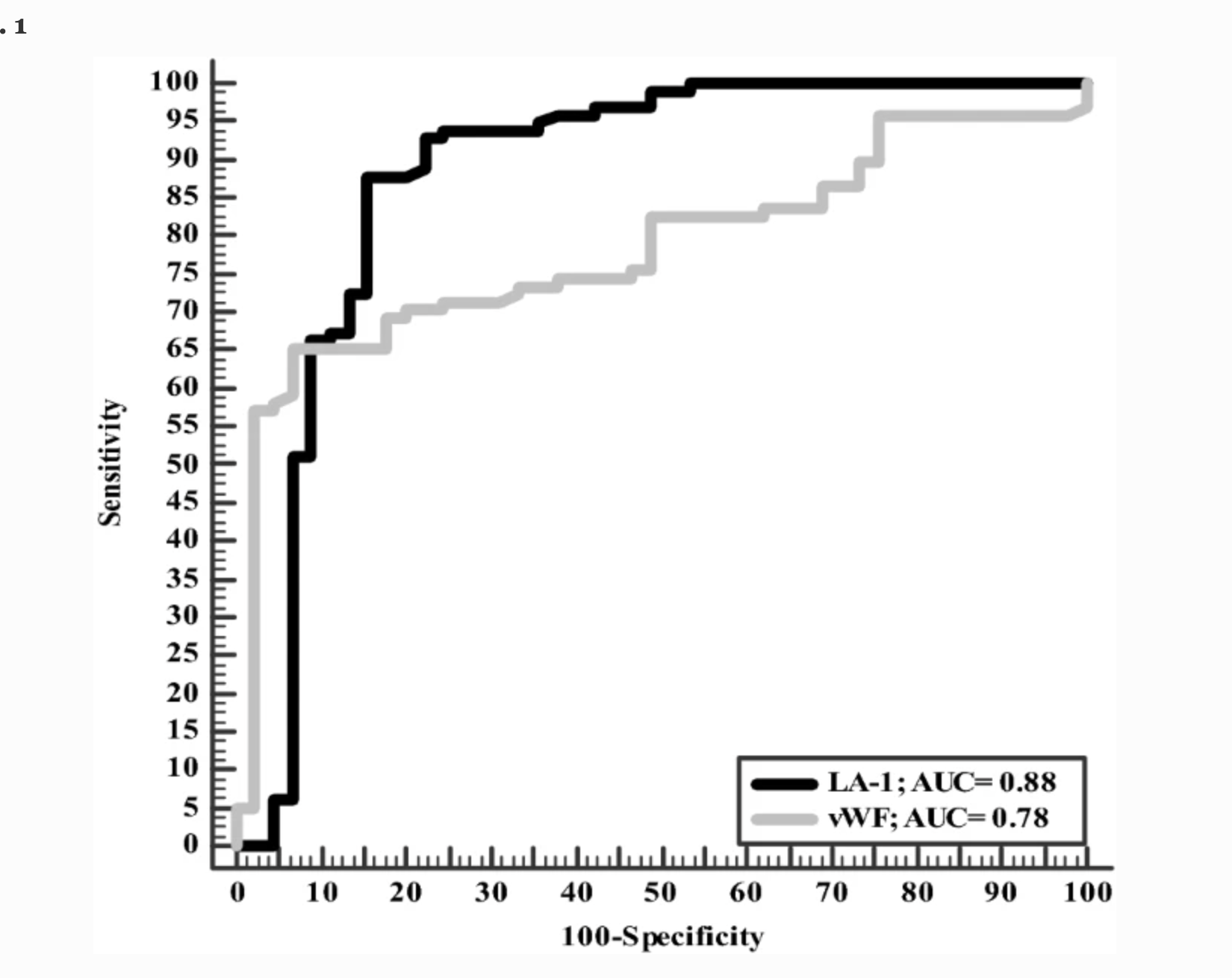
本项研究证实感染COVID-19病毒的患者易患不同形式的凝血病。这可能与不良结果有关。D-二聚体是诊断、严重程度评估而非血栓形成预测的主要工具。早期筛查这种并发症及其适当的管理将改善预后。
原始出处:
Azza Abdelaal. et al. Assessment of COVID -19 associated coagulopathy and multiple hemostatic markers: a single center study in Egypt. Infection.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













``丶1′家学习了
55
讲的很详细,学习懂了
56
不错学习了。
57
#期刊论坛##Nat#
0
不错的文章
45