Blood:用JAK1/2抑制剂治疗骨髓增生性肿瘤(MPN)可增加患者恶性B细胞淋巴瘤的发病率
2018-06-18 MedSci MedSci原创
抑制Janus激酶1/2(JAK1/2)是治疗骨髓增生性肿瘤(MPN)的主要方法。散发观察报道JAK1/2抑制剂治疗MPN过程中可共发B细胞非霍奇金淋巴瘤。Edit Porpaczy等人对626例MPN患者进行评估,其中包括69位采用JAK1/2抑制剂治疗的骨髓纤维化患者。69位采用JAK1/2治疗的患者中有4位(5.8%)进展成B细胞淋巴瘤,而采用常规治疗的557位患者中仅有2位(0.36%),
抑制Janus激酶1/2(JAK1/2)是治疗骨髓增生性肿瘤(MPN)的主要方法。散发观察报道JAK1/2抑制剂治疗MPN过程中可共发B细胞非霍奇金淋巴瘤。Edit Porpaczy等人对626例MPN患者进行评估,其中包括69位采用JAK1/2抑制剂治疗的骨髓纤维化患者。
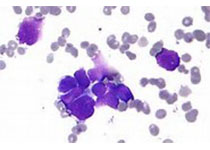
69位采用JAK1/2治疗的患者中有4位(5.8%)进展成B细胞淋巴瘤,而采用常规治疗的557位患者中仅有2位(0.36%),风险增加16倍。在另外一个独立的MPN患者(929位)队列中风险增加15倍。仅考虑原发性骨髓瘤患者(216位),31例抑制剂治疗的患者中有3位进展成淋巴瘤(9.7%),而对照的185位中仅1位(0.54%)。发生JAK2 V617F或其他MPN相关突变时,淋巴瘤呈侵袭性B细胞型、淋巴结外或白血病,伴有高MYC表达。
从开始抑制剂治疗到确诊淋巴瘤的中位时间是25个月。在16.3%的患者骨髓纤维化时的骨髓中检测到克隆性免疫球蛋白基因重组。在JAK1/2抑制剂治疗期间发展的淋巴瘤受已存在的B细胞克隆导向,在3位检测的患者中均是如此。
对2位患者进行测序验证了克隆基因的存在。Stat-/-小鼠可模拟JAK1/2抑制剂效应:16/24小鼠出现自发性髓系增生,并伴有异常B细胞。患病小鼠骨髓移植揭示恶性B细胞克隆生长进展成侵袭性B细胞白血病-淋巴瘤。
总而言之,本研究结果提示抑制骨髓纤维化个体的JAK/STAT1信号通路可增加侵袭性B细胞淋巴瘤的发病率。检测是否存在B细胞克隆或可鉴定高风险个体。
原始出处:
Edit Porpaczy,et al. Aggressive B-cell lymphomas in patients with myelofibrosis receiving JAK1/2 inhibitor therapy. Blood 2018 :blood-2017-10-810739; doi: https://doi.org/10.1182/blood-2017-10-810739
本文系梅斯医学(MedSci)原创编译,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#MPN#
0
#抑制剂#
29
#骨髓增生#
33
#发病率#
31
#细胞淋巴瘤#
28
看来治疗之后还要注意淋巴瘤发生
63
#JAK1/2抑制剂#
45
学习了,谢谢作者分享!
66
#增生性#
36
#2抑制剂#
37