莫西沙星:泌尿系感染能否适用?
2018-05-28 罗丽 成都市天府新区人民医院 SIFIC感染官微
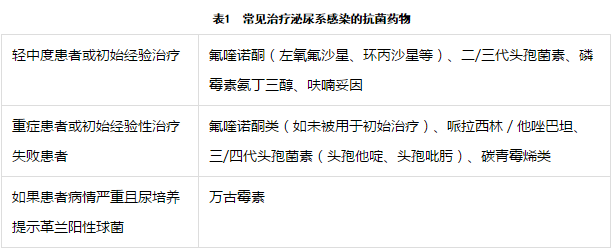
大家都知道,泌尿系感染根据是否有排尿机制功能和解剖结构异常(如尿路梗阻、尿流不畅、结石、尿路畸形、膀胱输尿管反流等)分为复杂性尿路感染和非复杂性尿路感染。尿路感染常见的细菌中百分之八十以上是阴性菌,大肠杆菌为主,百分之二十为阳性菌,肠球菌为主。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












行文风格幽默,好有意思!大致看懂了,学习!谢谢~
6
#莫西沙星#
126
学习了.谢谢分享!
92
学习了.谢谢分享
89
#泌尿系#
35
学习了谢谢分享
86
学习了.谢谢分享
91
学习了受益匪浅
67