Neurology-帕金森病,神经黑色素病变,影响运动or认知能力,解剖位置是重点!
2021-07-12 Freeman MedSci原创
神经黑色素病变,影响运动or认知能力,解剖位置是重点!
 蓝斑(locus coeruleus,LC)是位于桥脑的一个小核,它含有人脑中数量最多的产生去甲肾上腺素(NE)的神经元。它有广泛的投射到新皮层、下丘脑、小脑和大脑的其他部分,因此参与了一些神经生物学过程,包括记忆、执行功能、唤醒和调节睡眠周期和心脏功能。
蓝斑(locus coeruleus,LC)是位于桥脑的一个小核,它含有人脑中数量最多的产生去甲肾上腺素(NE)的神经元。它有广泛的投射到新皮层、下丘脑、小脑和大脑的其他部分,因此参与了一些神经生物学过程,包括记忆、执行功能、唤醒和调节睡眠周期和心脏功能。
LC去甲肾上腺素能系统的功能障碍,或导致精神和神经退行性疾病,包括帕金森病(PD)。与其生理功能一致,LC-NE系统的退化与帕金森病的非运动症状有关,即快速眼动睡眠行为障碍、抑郁症和认知能力下降。
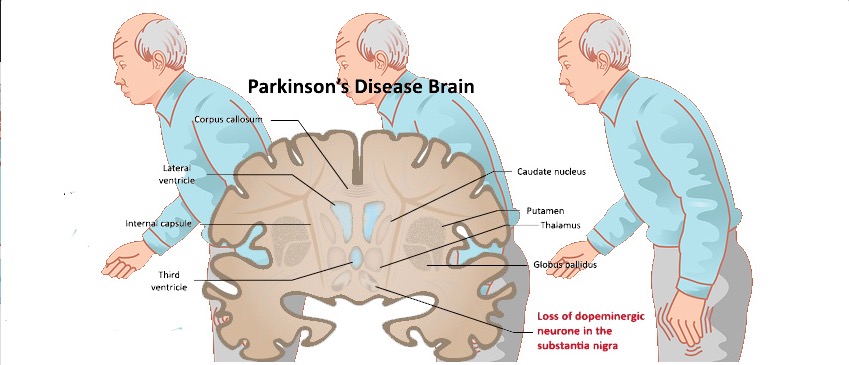
由于PD的神经病理过程从尾部脑干传播到LC,然后再传播到SN,LC-NE系统的变性通常先于黑质(SN)细胞的丧失,从而使疾病的运动表现出现。此外,PD的进展与认知能力下降有关,而认知能力下降是生活质量差的一个独立预测因素。在这种情况下,以前的尸检和动物研究表明,NE投射到前额叶皮质的损失有助于观察到PD患者的认知能力下降。
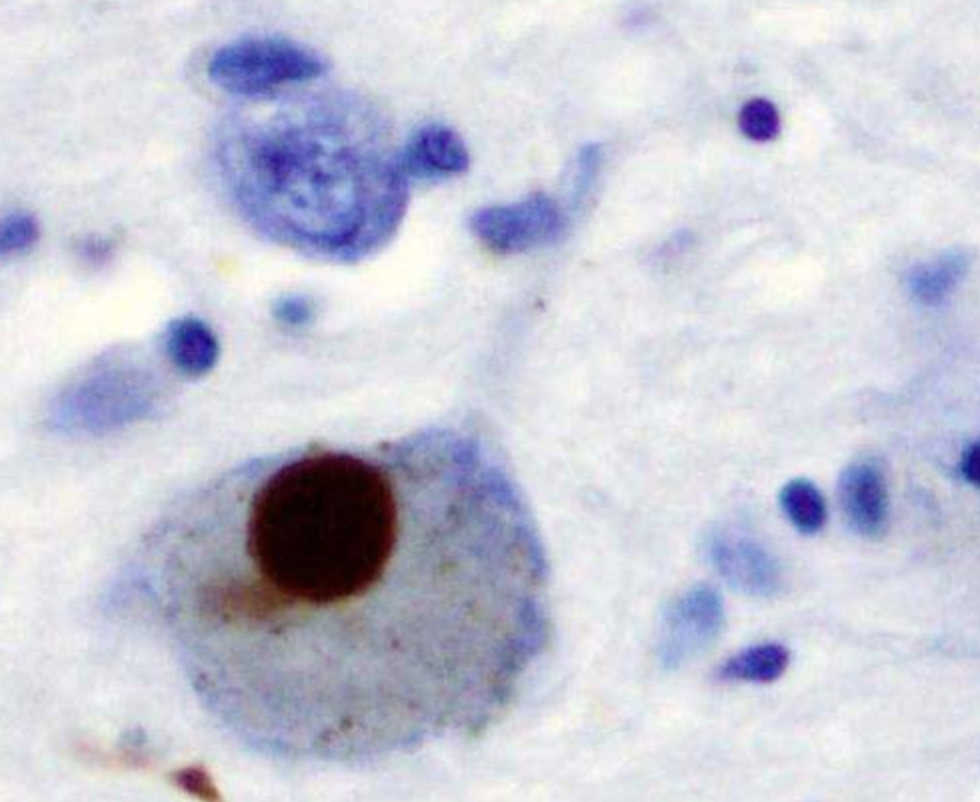
由于SN和LC的神经元在大脑中表现出最高浓度的神经黑色素(neuromelanin, NM),神经黑色素加权成像(NMI)提供了对PD病理生理学的探究思路。在NM中,铁可以在两个不同的部位结合,导致分子构型和离子亲和力的改变。这导致了松弛特性的改变,可以作为T1加权MRI扫描的对比。因此,NMI作为一种非侵入性的诊断方法出现,利用NM的顺磁特性,在NM丰富的区域提供明显的对比。因此,NMI可用于绘制SN和LC的神经元退化图,并可作为PD的一个有前途的生物标志物。
藉此,德国吕贝克大学的Jannik Prasuhn等人,提出假设L运动功能障碍与SN的NM水平降低有关,而认知能力下降与LC的NM水平降低有关。
他们对47名PD患者和53名匹配的对照组接受了运动评估、神经心理学测试和神经黑色素加权MRI。PD患者是在符合运动障碍协会临床诊断标准所定义的 "临床确立的PD "标准后被纳入的。两位独立的评分者对SN和LC进行鉴定,并计算对比度-噪声比(CNR)。
他们发现,与对照组相比,PD患者的SN和LC CNR均较低(p≤.001)。
SN的CNR而不是LC的CNR与病程密切相关(p<0.001)。含有背外侧SN的神经黑色素病变与MDS-UPDRS I、II和III相关,但与认知功能无关。
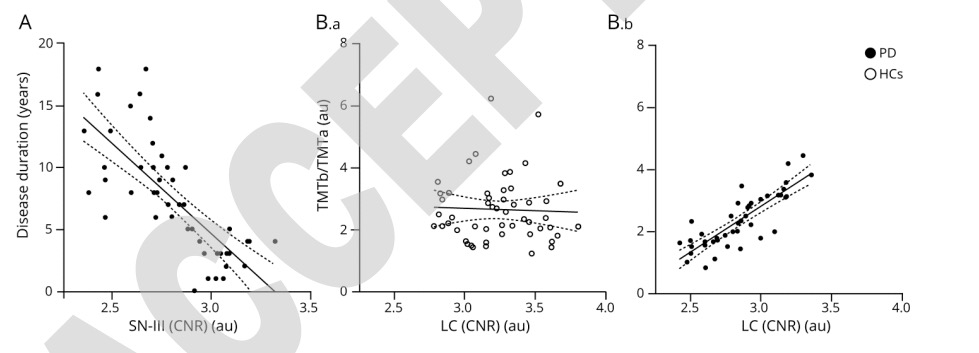 相反,LC的神经黑色素病变与所有测试领域的认知功能有关,但与运动障碍或日常生活活动无关。对照组中没有这种关联。
相反,LC的神经黑色素病变与所有测试领域的认知功能有关,但与运动障碍或日常生活活动无关。对照组中没有这种关联。
这个研究的重要意义在于:发现了SN和LC的神经黑色素成像非常适用于绘制PD的神经变性图。SN的神经黑色素病变与运动功能障碍相关,而LC的病变则与认知障碍相关。因此,LC的神经黑色素加权成像可以作为PD的执行和其他认知功能障碍的成像标志物。
原文出处:
Prasuhn J, Prasuhn M, Fellbrich A, Strautz R, Lemmer F, Dreischmeier S, Kasten M, Münte TF, Hanssen H, Heldmann M, Brüggemann N. Association of Locus Coeruleus and Substantia Nigra Pathology With Cognitive and Motor Functions in Patients With Parkinson Disease. Neurology. 2021 Jun 29:10.1212/WNL.0000000000012444. doi: 10.1212/WNL.0000000000012444. Epub ahead of print. PMID: 34187859.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Neurol#
30
#色素#
32
赞
47
#黑色素#
43
#黑色素#
33