Movement Disorders:2型糖尿病或是帕金森氏病风险和进展的决定因素
2021-03-10 MedSci原创 MedSci原创
糖尿病(DM)被世界卫生组织(WHO)认为是四大非传染性疾病之一。据国际糖尿病联合会(IDF)2019年数据预测,到2045年,全球糖尿病患者将增长51%,达到7亿。
糖尿病(DM)被世界卫生组织(WHO)认为是四大非传染性疾病之一。据国际糖尿病联合会(IDF)2019年数据预测,到2045年,全球糖尿病患者将增长51%,达到7亿。然而,随着科学家对DM的认识不断加深,诸多证据表明,2型糖尿病(T2DM)和帕金森氏病(PD)之间存在紧密的关联性,两者都以异常的蛋白质积累、溶酶体和线粒体功能障碍以及慢性系统性炎症为特征。胰岛素抵抗是T2DM的标志,也可能是导致PD的重要因素。
先前系统性评价和荟萃分析结深入探讨过有关T2DM和PD之间的风险关系,但结果不一致。近日,发表在Movement Disorders杂志的一项研究显示,T2DM可促进PD的发生发展,且可能有助于加快PD的认知衰退。同时,治疗T2DM可能会减缓PD的进展。

在这项研究中,研究人员通过检索6个数据库,包括PubMed,Web of Science,Scopus,Ovid,bioRxiv和medRxiv,共收集了33408篇文章,其中选取28篇高质量研究进行荟萃分析,调查T2DM与PD风险和进展的关联。检索时间为2020年6月2日至2020年6月6日,检索时所用的术语为“ 2型糖尿病”和“帕金森氏病”或“ 2型糖尿病”和“帕金森氏病进展”或“ 2型糖尿病”和“帕金森氏病风险”。纳入的主要荟萃分析的研究包括(1)观察性研究:调查T2DM对PD发病风险的影响;(2)糖尿病与PD进展相关的研究。之后,使用孟德尔随机化(MR),利用来自全基因组关联研究的汇总数据,对T2DM和PD风险和进展的因果关系进行探索。
结果显示,在最高质量的前瞻性研究中,T2DM对PD发生发展风险的影响最明显,并且有一些证据表明,T2DM可加快认知能力下降。在使用MR分析中,研究发现T2DM与PD发病风险可能存在因果关系,T2DM可能会增加PD的运动发展速度,但对认知发展的影响的支持较弱。
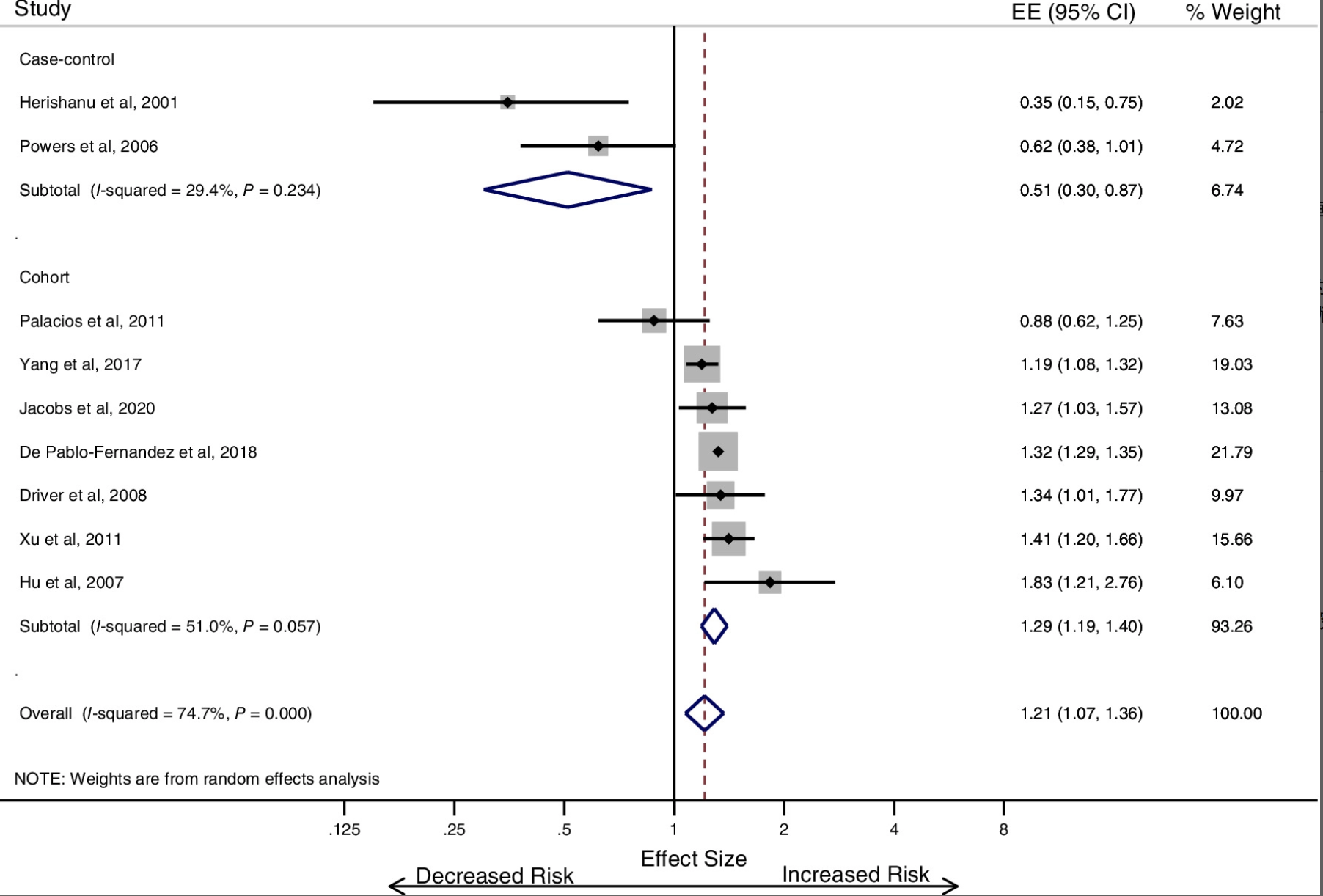
2型糖尿病与帕金森氏病发展风险增加相关
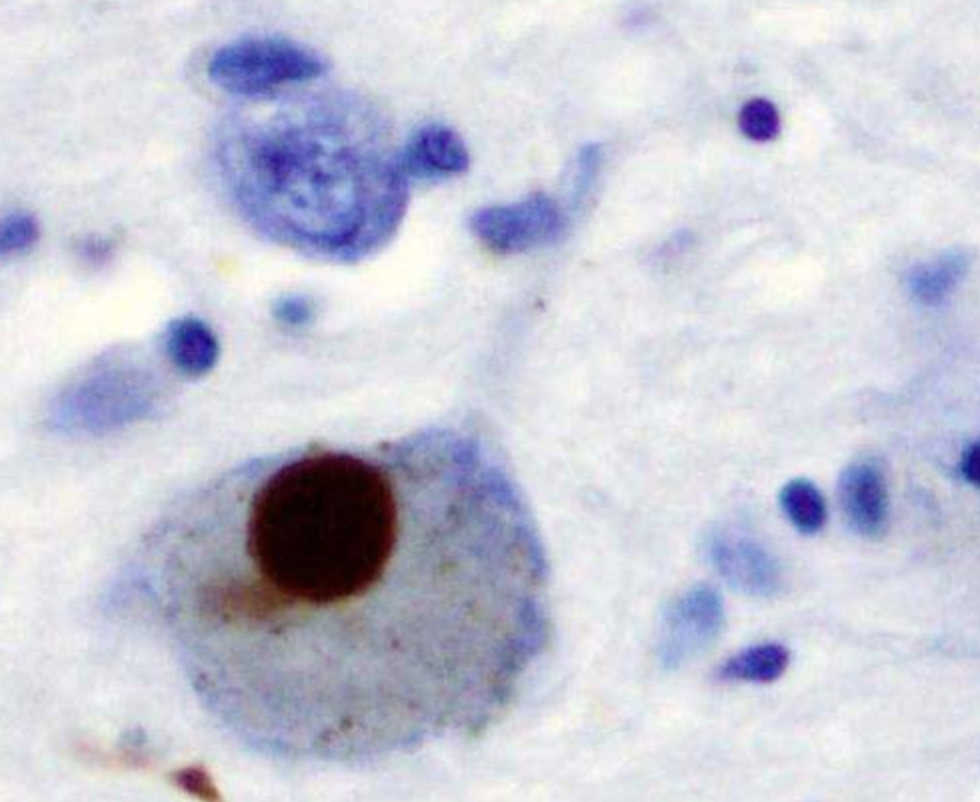
T2DM和PD之间共享生物学的证据越来越多。在T2DM中,胰岛淀粉样多肽(IAPP)或胰岛淀粉样多肽在胰腺细胞中聚集形成淀粉样斑块。同样,PD在病理上是由神经元内α-突触核蛋白的积累定义的。一些证据表明,在存在IAPP的情况下,PD中α-突触核蛋白的聚集发生得更快。
总之,该研究结果证明T2DM不仅影响PD的发病风险,而且还影响PD的进展。此外,许多用于治疗T2DM的方法策略,可能将其重新用于治疗PD,建议PD进行T2DM的筛查和早期治疗。
原始出处
Harneek Chohan et al, Type 2 Diabetes as a Determinant of Parkinson's Disease Risk and Progression, Movement Disorders (2021). DOI: 10.1002/mds.28551
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Disord#
26
#disorders#
36
#决定因素#
52
#disorder#
31
#ERS#
29
#Dis#
24
谢谢MedSci提供最新的资讯
43