JCC: 维生素D与炎症性肠病患者体内α4β7+免疫表型相关并可以预测维多珠单抗治疗失败概率
2021-06-29 MedSci原创 MedSci原创
整合素α4β7是促进白细胞运输到肠道,导致肠道炎症产生的重要粘附分子。
整合素α4β7是促进白细胞运输到肠道,导致肠道炎症产生的重要粘附分子。维多珠单抗是一种针对α4β7 的人源化单克隆抗体,主要用于炎症性肠病的治疗。但是只有约40%的患者会获得临床缓解,很大一部分患者随着时间的推移而逐渐失去对药物的反应。维多珠单抗失败的潜在机制尚不清楚。维生素D水平是一个公认的与炎症性肠病有关的危险因素,维生素 D 受体 (VDR) 的遗传多态性与溃疡性结肠炎和克罗恩病的疾病易感性存在相关性。有研究显示维生素D能下调免疫细胞上整联蛋白α4β7 的表达。因此,本项研究旨在探究维生素D与α4β7 免疫表型和 IBD 中维多珠单抗治疗失败风险相关性。

研究人员使用质谱流式细胞术 (CyTOF) 对未使用维多珠单抗的 IBD 患者(N = 48)进行了外周和肠道免疫细胞的单细胞免疫表型分析。同时研究人员分析了来自 GEMINI I 和 GEMINI 长期安全性 (LTS) 的全基因组粘膜基因表达 (GSE73661),以确定维生素 D 受体 (VDR) 与整合素α-4 (ITGA4) 和β-7 (ITGB7) 基因之间的关联. 最后研究人员在回顾性和前瞻性 IBD 队列(N = 252)中使用逻辑回归估计了治疗前维生素D水平较低的维多珠单抗治疗失败的几率。
免疫表型分析显示,较高的25(OH)D水平与α4β7+外周血单核细胞(R=-0.400,P<0.01)和α4β7+肠道白细胞(R = -0.538,P=0.03)减少有关。血清 25(OH)D水平与α4β7+外周 B 细胞和自然杀伤 (NK) 细胞以及 α4β7+肠道B细胞、NK细胞、单核细胞和巨噬细胞呈负相关关系。VDR的粘膜表达与 ITGA4 和 ITGB7 表达呈负相关关系。在多变量分析中,25(OH)D<25ng/mL 与诱导期间维多珠单抗无反应应答相关(OR 26.10,95% CI 14.30-48.90,P<0.001)也和1年随访失败几率增加相关(OR 6.10,95% CI 3.06-12.17,P<0.001)。
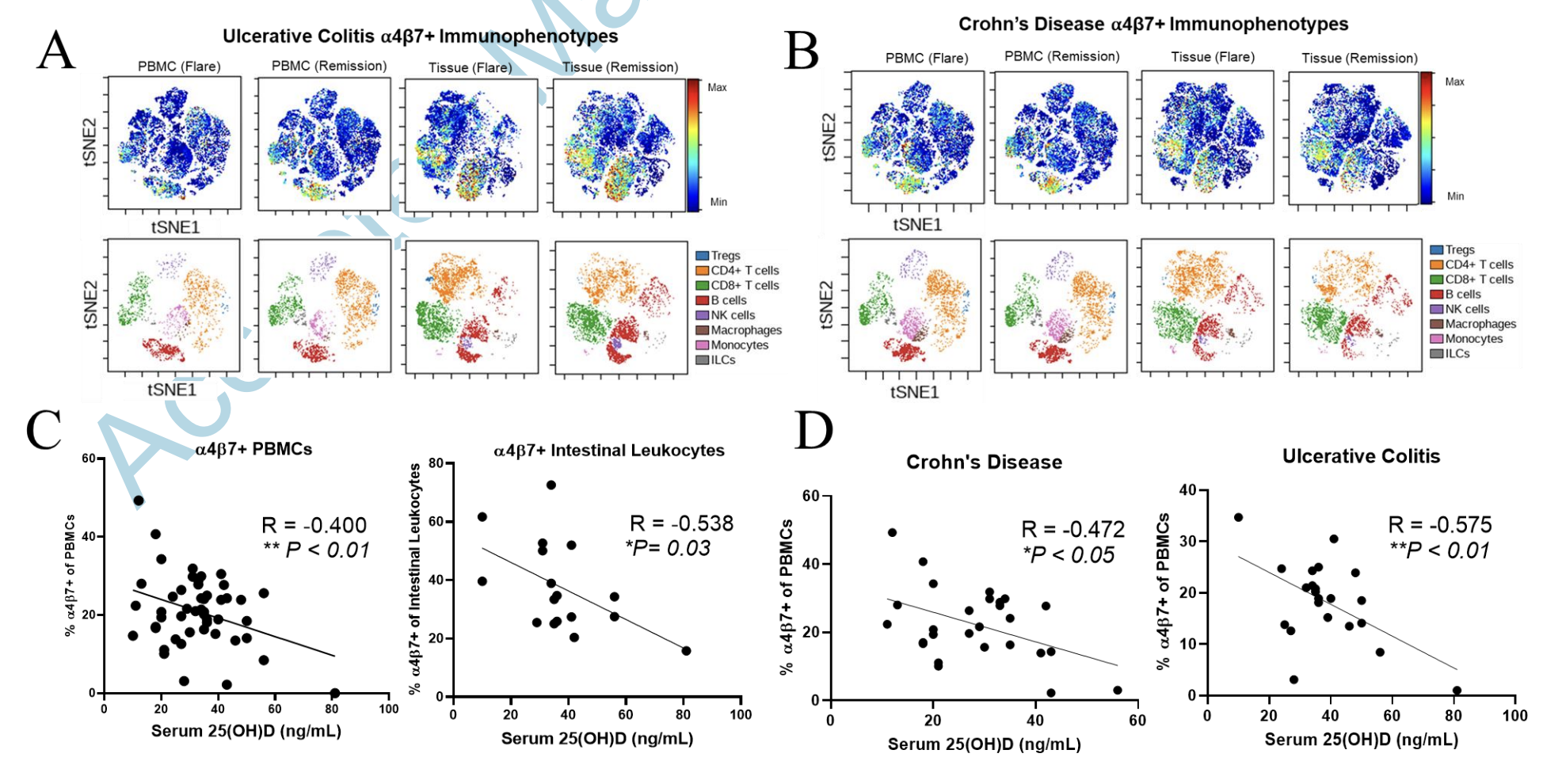
图:α4β7+免疫表型与维生素D水平的关系
因此,通过本项研究证实低血清25(OH)D水平与α4β7+免疫表型相关,也可以预测IBD患者未来的维多珠单抗失败概率。
原始出处:
John Gubatan. Et al. Vitamin D is Associated with α4β7+ Immunophenotypes and Predicts Vedolizumab Therapy Failure in Patients with Inflammatory Bowel Disease. Journal of Crohn's and Colitis.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#治疗失败#
48
#表型#
35
#炎症性#
28
#炎症性肠病患者#
0