Am J Rhinol Allergy:过敏性鼻炎患者外周血嗜碱性粒细胞中Toll-Like受体7的表达上调
2021-02-21 AlexYang MedSci原创
之前有报道称,Toll样受体7(TLR7)激动剂可以通过促进Th1细胞因子的释放和抑制Th2细胞的功能来改善过敏性鼻炎(AR)的症状。然而,对TLR7在AR嗜碱性细胞中的表达知之甚少。
之前有报道称,Toll样受体7(TLR7)激动剂可以通过促进Th1细胞因子的释放和抑制Th2细胞的功能来改善过敏性鼻炎(AR)的症状。然而,对TLR7在AR嗜碱性细胞中的表达知之甚少。
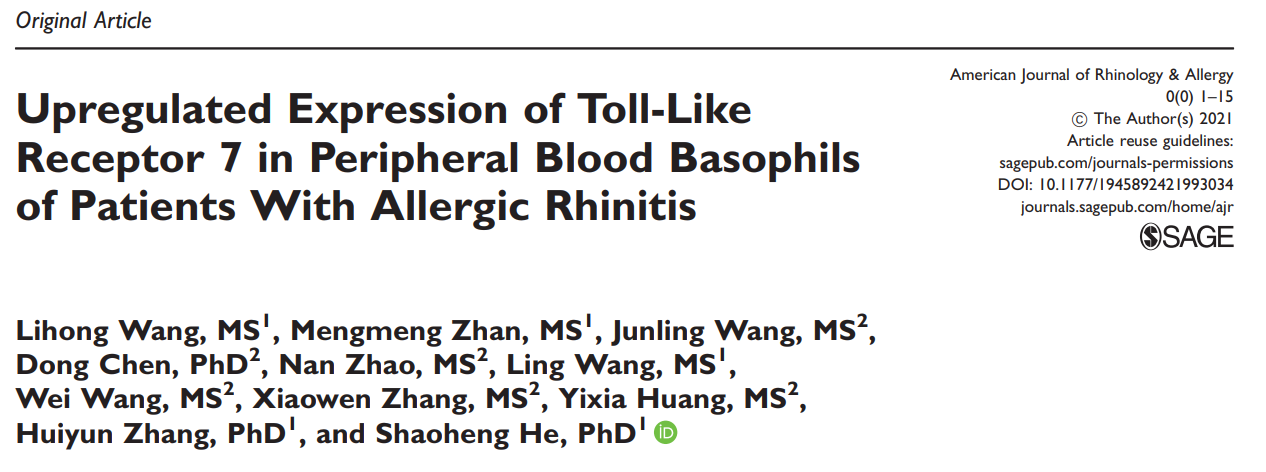
最近,有研究人员调查了TLR7在AR嗜碱性细胞中的表达,以及过敏原对TLR7表达的影响。研究发现,与健康对照(HC)受试者相比,AR患者血粒细胞和单核细胞群中TLR7+CCR3+细胞(P<0.001,P=0.011)、TLR7+CD123+HLA-DR-细胞(P=0.016,P=0.042)和TLR7+CCR3+CD123+HLA-DR-细胞(P=0.046,P=0.035)的百分比均增加;另外,CCR7 MFI对CCR3+细胞(P=0.050和P=0.043)、CD123+HLA-DR-细胞(P<0.001和P=0.002)和CCR3+CD123+HLA-DR-细胞(P<0.001和P=0.003)的作用增强。过敏原Der p1和OVA在KU812细胞中引发TLR7在蛋白和mRNA水平表达上调和IL-13的产生。屋尘螨提取物(HDME)、大籽蒿野生过敏原提取物(ASWE)、IL-31、IL-33、IL-37和TSLP在孵育2 h后诱导KU812细胞IL-6释放升高。
KU812细胞中TLR7表达的流式细胞分析
最后,研究人员指出,AR患者血液中TLR7+嗜碱性粒细胞的比例和单个嗜碱性粒细胞中TLR7的表达强度均升高,表明嗜碱性粒细胞很可能通过TLR7参与AR的发病过程。
原始出处:
Lihong Wang , Mengmeng Zhan , Junling Wang et al. Upregulated Expression of Toll-Like Receptor 7 in Peripheral Blood Basophils of Patients With Allergic Rhinitis. Am J Rhinol Allergy. Feb 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#过敏性#
20
#Toll-like#
35
#ALL#
29
#外周血#
32
#嗜碱性粒细胞#
23