Annals of Neurology:癫痫样活动峰值负荷自动测量可能改善癫痫患者预后
2021-10-28 MedSci原创 MedSci原创
癫痫样活动峰值负荷的自动测量为未来的多中心随机试验提供了一个方便、一致和可量化的目标,以研究抑制癫痫样活动是否能改善结果。
在接受脑电图(EEG)脑监测的危重病患者中,多达一半的患者出现癫痫样周期性和节律性脑活动(癫痫样活动[EA])。这些模式已被证明与神经功能残疾和死亡率增加相关,随着不良结局的概率与EA的负担成比例增加。
Sahar F. Zafar等开发了一种新的自动化方法,能够有效地对急性病住院患者的大量连续脑电图记录中的所有癫痫样模式进行注释。利用这些注释,开发了一个机器学习模型来估计出院时持续暴露于EA对神经功能残疾水平的独立贡献。该研究文章发表在Annals of Neurology杂志。
该研究旨在确定急性病患者癫痫样活动负荷与预后之间的剂量-反应关系。Sahar F. Zafar等采用单中心回顾性分析方法,对1967例神经科、内科和外科患者进行回顾性分析,这些患者在2011年至2017年间接受了16小时以上连续脑电图(EEG)。该研究小组开发了一种人工智能算法来注释11.02 tb的脑电图,并在记录后72小时内量化癫痫样活动负荷。评估了(1)在记录的前24小时内的负荷,(2)在负荷最高的12小时内(峰值负荷)的负荷,(3)在监测的前72小时内累积的负荷。采用机器学习评估癫痫样负担对结果的影响。结果衡量标准为出院改良Rankin量表,分为良好(0-4)和较差(5-6)。

正常脑电图(EEG)、发作和周期型发作的示例。每幅脑电图图像都显示了一个10秒的纵向双极蒙太奇记录片段。
正常脑电图(EEG)、发作和周期型发作的示例。每幅脑电图图像都显示了一个10秒的纵向双极蒙太奇记录片段。
Sahar F. Zafar等癫痫样负荷峰值与不良结局独立相关(p < 0.0001)。其他独立的关联包括年龄、急性生理学和慢性健康评估II评分、癫痫发作和缺氧缺血性脑病的诊断。根据最后一次脑电图测量(监测72小时以内)到放电的时间间隔计算3层模型校准误差:(1)最后一次脑电图测量到放电的时间间隔<5天,0.0941(95%置信区间[CI] = 0.0706-0.1191);最后一次测量到出院为5 - 10天,0.0946 (95% CI = 0.0631-0.1290);最后一次测量到放电为10天,0.0998 (95% CI = 0.0698-0.1335)。校正协变量后,癫痫样活动负荷峰值从0增加到100%,不良结局的概率增加了35%。
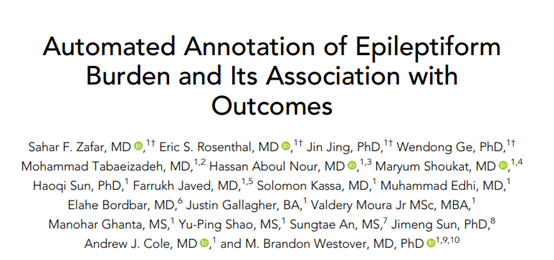
首次24小时癫痫样活动(EA)负荷。
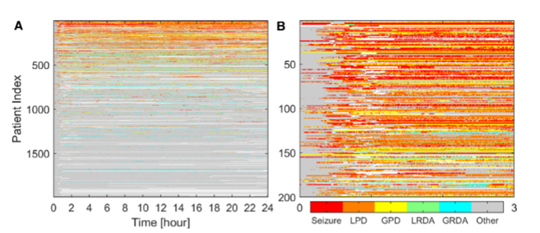
亚组分析中癫痫样活动负荷和预后之间的剂量-反应关系。
上图中(A)在急性脑损伤(ABI)患者中,与癫痫样活动峰值(EA)负荷为0%和100%的患者相比,预后不良的概率增加了20%到30%。(B)在缺氧缺血性脑病(HIE)患者中,与EA峰值负荷为0%和100%的患者相比,不良预后的概率增加了60%到70%。(C)在急性发作/癫痫持续状态(SZ/SE)患者中,与峰值EA负荷为0%和100%的患者相比,不良结局的概率增加了50%。(D)在原发性全身疾病患者中,与EA峰值负荷为0%和100%的患者相比,不良结局的概率增加10%到20%。
癫痫样活动峰值负荷的自动测量为未来的多中心随机试验提供了一个方便、一致和可量化的目标,以研究抑制癫痫样活动是否能改善结果。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#自动测量#
52
#癫痫患者#
40
#Neurol#
33
#患者预后#
30