血检无异常的酒后腹痛,背后暗藏“杀机”!| Medscape病例分享
2018-12-30 放生蓮(编译) 中国医学论坛报
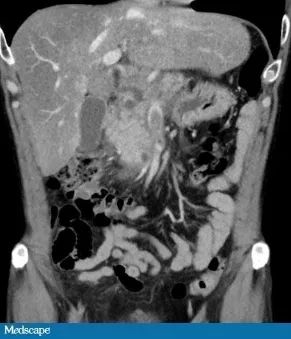
酒后腹痛,你首先会想到什么?很多临床医生会说:急性胰腺炎。没错,但是除此之外,还有很多其他罕见原因,比如下面这个饮酒引起的的腹痛案例,可以说是“暗藏玄机”!


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#PE#
27
#CAP#
32
#腹痛#
34
#SCAP#
32
#血检#
45
#Medscape#
26
#Med#
31