Dig Dis Sci:炎症性肠病疾病活动和表型对孕前和孕妇生活质量的影响
2022-08-19 xuyihan MedSci原创
炎症性肠病,是病灶累及回肠、直肠、结肠的一种特发性肠道的炎症性疾病。临床常见表现为腹泻、腹痛。
炎症性肠病 (IBD)主要包括克罗恩病 (CD) 和溃疡性结肠炎 (UC),是一种与令人非常痛苦的慢性复发性炎症性疾病。IBD最常在青春期和青年期被诊断出来,它会影响患者的自尊、心理健康和身体形象。而患有IBD的育龄妇女在应对妊娠和 IBD 之间的相互作用方面面临着额外的挑战。患有 IBD 的女性更可能没有孩子,在CD和UC患者中的发生率分别为18%和14%,而在普通人群中为6.2%,这种现象被认为是适龄期妇女对妊娠期IBD治疗的误解和恐惧。
健康相关的生活质量 (HRQoL) 量表是一种经过验证的评估IBD患者生活质量的工具。IBD 相关的 HRQoL 受到疾病活动的极大影响,因此,评估 IBD 孕妇 HRQoL 的预测因素对于制定优化孕期HRQoL和IBD管理的策略至关重要,目前尚不清楚IBD相关 HRQoL如何在孕前(PC)、妊娠和产后的不同时间点受到影响。因此,本项研究旨在前瞻性评估 IBD 女性从 PC 到产后的纵向变化。
研究人员在一家三级转诊中心对孕前到产后12个月内的IBD孕妇患者进行了前瞻性研究。参与者完成了简短的IBD问卷 (SIBDQ),并评估了临床疾病活动性(改良的 Harvey Bradshaw 指数或Mayo评分)和客观疾病活动性(C反应蛋白 [CRP]、粪便钙卫蛋白 [FCP])。

本项研究最后共纳入61名IBD患者(25名CD,36名UC)。研究结果显示在孕前,UC 患者的 SIBDQ 肠道和社交评分高于CD患者,但在产后发生逆转。患有CD而不是UC的患者在怀孕后SIBDQ出现显着的改善,这种改善持续到产后12个月。在多变量线性回归模型中,临床疾病活动对每个妊娠时间点和产后 12 个月的 SIBDQ都有负性预测作用。同时研究人员发现CRP≥8.0mg/L 的患者在妊娠1个月 (T1) 期间的SIBDQ显着降低,但在妊娠后期不显着。FCP≥250mg/kg的患者在 T2、T3 和产后6个月时的SIBDQ评分显着降低。
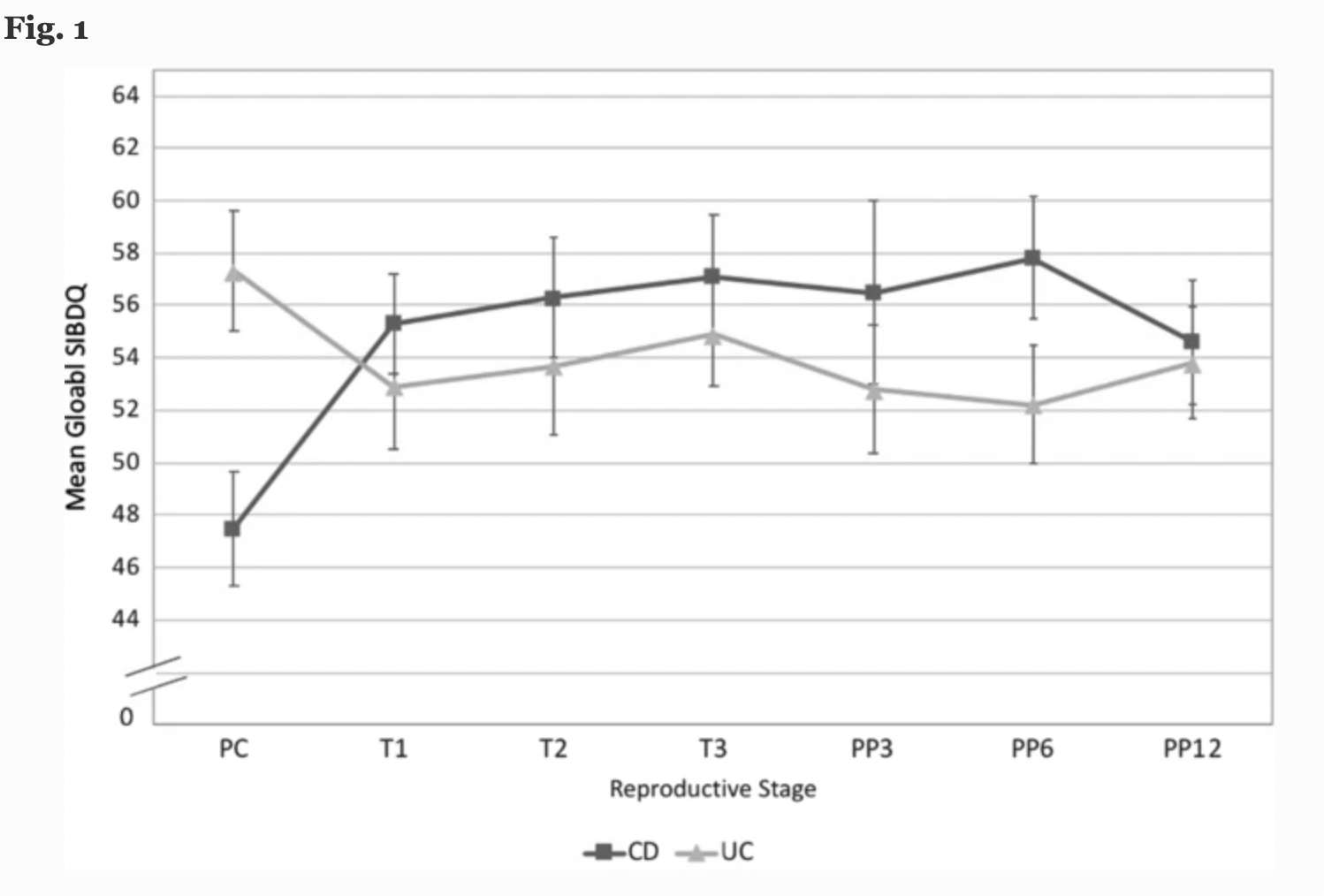
本项研究证实临床疾病活动是从IBD孕妇受孕到产后12个月生活质量的负预测因子。UC 患者的孕前 HRQoL 更好,但产后 HRQoL比CD患者更差。
原始出处:
Grace Wang. et al. Impact of Disease Activity and Inflammatory Bowel Disease Subtype on Quality of Life in Preconception and Pregnant Patients. Digestive Diseases and Sciences.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Dis#
36
#疾病活动#
38
#孕前#
43
#表型#
41
#炎症性#
49