NPJ Biofilms Microbiomes:血液透析患者的肠道菌群失调与死亡率。
2021-03-18 MedSci原创 MedSci原创
肠道微生物多样性和组成与接受维持性血液透析的ESKD患者的全因死亡率密切相关。炎症可能参与了肠道生物失调的发病机制。
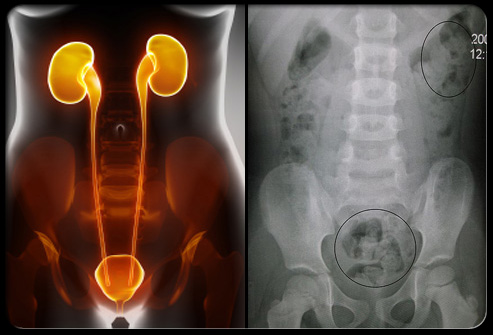
接受透析的终末期肾病(ESKD)患者的预期寿命比普通人群明显缩短。心血管疾病(CV)和非心血管疾病的死亡风险都同样增加。确定与这一较高风险相关的因素对ESKD患者的护理很重要。对透析患者的观察性研究指出了更大死亡风险的几个预测因素,包括高龄和高发病率,特别是糖尿病(DM)和心血管疾病(CVD)(传统危险因素)、营养不良、炎症和尿毒症溶质积累(非传统危险因素)。
越来越多的研究表明,肠道微生物区系对于抵御病原体和维持正常的免疫和代谢稳态至关重要。健康的人体胃肠道含有高度多样化的微生物种群。相反,尿毒症会改变肠道微生物区系的正常组成和功能,通常被称为肠道生物失调。肠道生物失调促进局部和全身性炎症,从而导致各种病理后果。越来越多的证据也表明肠源性尿毒症毒素参与了ESKD脑血管病的发病机制。
肠道生物失调的特征是多样性的丧失和组成的失衡。高α多样性(衡量细菌丰富度和均匀性的指标)通常与更好的健康状况有关。在接受异基因造血细胞移植的患者和因慢性阻塞性肺疾病住院的患者中,已经描述了微生物多样性降低与生存不良的关系。有研究发现营养不良和炎症与ESKD患者肠道微生物多样性显著降低有关。然而,目前尚不清楚肠道微生物多样性降低是否与ESKD的不良后果有关。有研究探索肠道生物失调是否可以预测ESKD死亡风险,并进一步分析死亡者和幸存者的肠道微生物区系,研究成果发表在NPJ Biofilms Microbiomes杂志。

慢性肾脏疾病患者的肠道生物失调、炎症和不良后果之间的关系知之甚少。该研究分析了血液透析患者中微生物多样性与全因死亡率的关系。采用16S核糖体RNA基因测序分析肠道微生物区系。在中位数2.1年的随访中,多样性较高(中位数以上)的患者调整后的死亡风险比多样性较低(中位数以下)的患者低74%。然后,比较了死亡者和幸存者之间的微生物组成。观察到死亡患者的微生物多样性明显低于幸存者,而促炎细胞因子明显高于幸存者。具体地说,死亡患者体内产生短链脂肪酸的两种短链脂肪酸细菌-蔗糖弧菌(Succinivibrio)和厌氧菌(AnAerostipes)的相对丰度明显降低。因此,一种独特的肠道微生物组成与血液透析患者死亡风险的增加有关,可用于识别预后不良的受试者。
总之,这项研究表明肠道微生物多样性和组成与接受维持性血液透析的ESKD患者的全因死亡率密切相关。炎症可能参与了肠道生物失调的发病机制。未来的研究需要更大的样本量和更长的随访时间来验证我们的观察结果,并调查针对特定微生物靶点的干预是否会改变血液透析患者的结果。
原文出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#CRO#
52
#Microbiome#
41
#Bio#
36
#Micro#
0
学习了
70
学习了
69
#血液透析#
45
#肠道菌#
45
#透析患者#
59
#MES#
44