Clin Cancer Res:醋酸阿比特龙通过诱导CREB1磷酸化和增强CBP-p300复合物的功能导致前列腺癌细胞产生耐药
2021-02-09 AlexYang MedSci原创
醋酸阿比特龙(AA)是CYP17A1的抑制剂,是FDA批准的治疗晚期前列腺癌的药物。然而,并非所有患者都对AA有响应,最初有反应的患者最终也会产生AA耐药性。最近,有研究人员确定了前列腺癌细胞的AA耐
醋酸阿比特龙(AA)是CYP17A1的抑制剂,是FDA批准的治疗晚期前列腺癌的药物。然而,并非所有患者都对AA有响应,最初有反应的患者最终也会产生AA耐药性。最近,有研究人员确定了前列腺癌细胞的AA耐药机制。
研究结果发现,耐药细胞系在没有药物选择的情况下,表型稳定,并表现出永久性的全局基因表达变化。磷酸化的CREB1(pCREB1)在AA耐药细胞系中增加,是控制全局基因表达的关键。pCREB1的上调使前列腺癌细胞对AA不敏感,而阻断CREB1的磷酸化能够使AA耐药细胞对AA重新敏感。AA治疗会增加细胞内cAMP水平,诱导激酶活性,并导致CREB1的磷酸化,随后可能增强CBP/p300复合物在AA耐药细胞中的重要作用,因为AA耐药细胞对CBP/p300抑制剂表现出相对更高的敏感性。进一步的药代动力学研究表明,AA与CBP/p300抑制剂在限制前列腺癌细胞生长方面具有显著的协同作用。
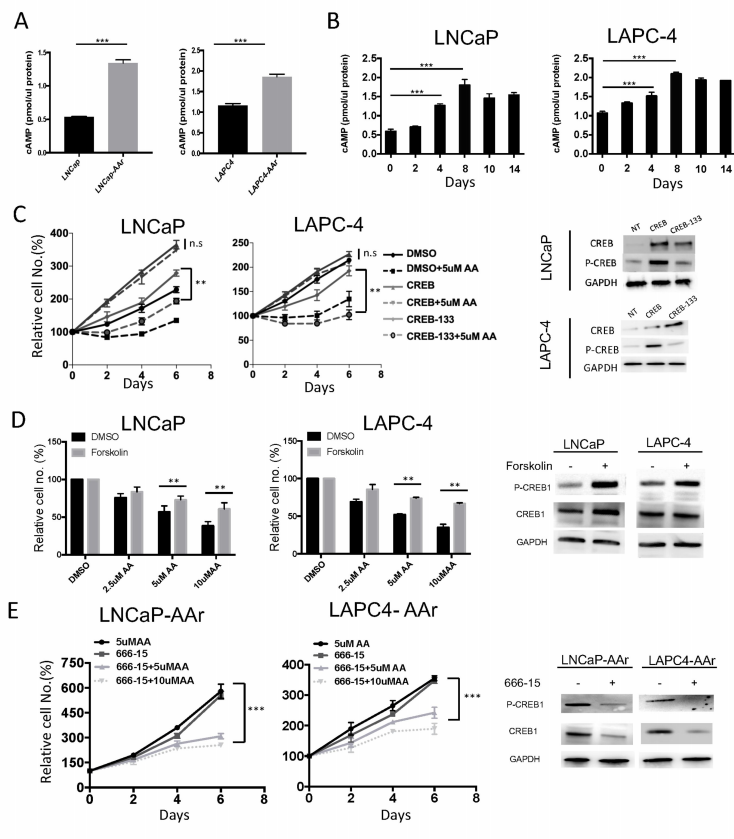
前列腺癌细胞系中CREB1激活能够使得AA治疗去敏化
最后,研究人员指出,AA治疗能上调pCREB1,从而增强CBP/p300的活性,导致全局性的基因表达改变,并随后导致耐药性的产生。因此,将AA与靶向耐药机制的疗法相结合,可能会产生更有效的治疗策略。
原始出处:
Wenting Pan, Zhouwei Zhang, Hannah Kimball et al. Abiraterone acetate induces CREB1 phosphorylation and enhances the function of the CBP-p300 complex, leading to resistance in prostate cancer cells. Clin Cancer Res. Jan 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#复合物#
55
#CBP#
50
#癌细胞#
35
#醋酸阿比特龙#
46
#CRE#
49
#前列腺癌细胞#
40
前列腺癌相关研究,学习了,谢谢梅斯
57