JAMA子刊:乳腺癌远处淋巴结转移可能是一种区域性疾病,可从局部治疗中获益
2021-03-17 MedSci原创 MedSci原创
远处淋巴结转移(DLNM)与同侧锁骨上淋巴结转移(ISLM)患者的生存率和其他Ⅳ期乳腺癌患者不同吗?
乳腺癌是世界范围内常见的恶性疾病。新诊断的乳腺癌患者同时发生远处转移的发生率约为3%至8%。全身治疗是Ⅳ期乳腺癌的主要治疗方法,可以延长患者生存期,减轻症状。然而,随着全身治疗的进展,高度选择性的IV期乳腺癌(如骨或远处淋巴结转移的患者)可能是可治愈的,特别是对于转移局限或有利部位的病例。了解乳腺癌转移的特点对选择合适的患者进行精确、积极的治疗是必要的。

pixabay.com
以往的研究表明,区域淋巴结转移本身是不致命的,但可以指示远处器官的转移和预后。然而,关于淋巴结转移在疾病进一步进展中的作用仍存在激烈的争论。有研究认为淋巴结转移具有播散远端器官的潜能,然而,其他研究认为局部淋巴结转移在临床上并不重要。至于淋巴结转移患者与其他类型的IV期乳腺癌患者在预后和治疗上是否存在差异,还需要进一步的探索。
对于远处淋巴结转移(DLNM)与同侧锁骨上淋巴结转移(ISLM)患者的生存率和其他Ⅳ期乳腺癌患者的生存率是否不同,目前尚缺乏研究。基于这些背景理论,有研究者对此进行了相关研究,研究结果近日发表在JAMA子刊患者的生存率JAMA Network Open期刊上。

这项队列研究包括2010年1月1日至2014年12月31日期间,从监测、流行病学和最终结果登记数据库中纳入的诊断为的乳腺癌的2033名患者。包括三组患者:(1)无远处转移的ISLM患者,(2)DLNM患者,(3)有远处转移患者(DLNM除外)。年龄小于18岁或大于100岁的患者被排除在外。数据分析于2020年2月。主要终点为总生存期(OS)和乳腺癌特异性生存期(BCSS)。
在纳入的2033名患者中,346名患者(17.0%)有DLNM,212名患者(10.4%)有ISLM,1475名患者(72.6%)有远处转移(DLNM除外)。ISLM组3年BCSS发生率为63.24%,DLNM组为64.54%,远处转移组为41.20%。3年生存率ISLM为53.46%,DLNM为62.67%,远处转移为38.21%。与ISLM患者相比,DLNM患者的BCSS和OS相似,而远处转移患者的BCSS和OS明显较差。在346例DLNM患者中,初次手术和放疗与OS的改善显著相关。
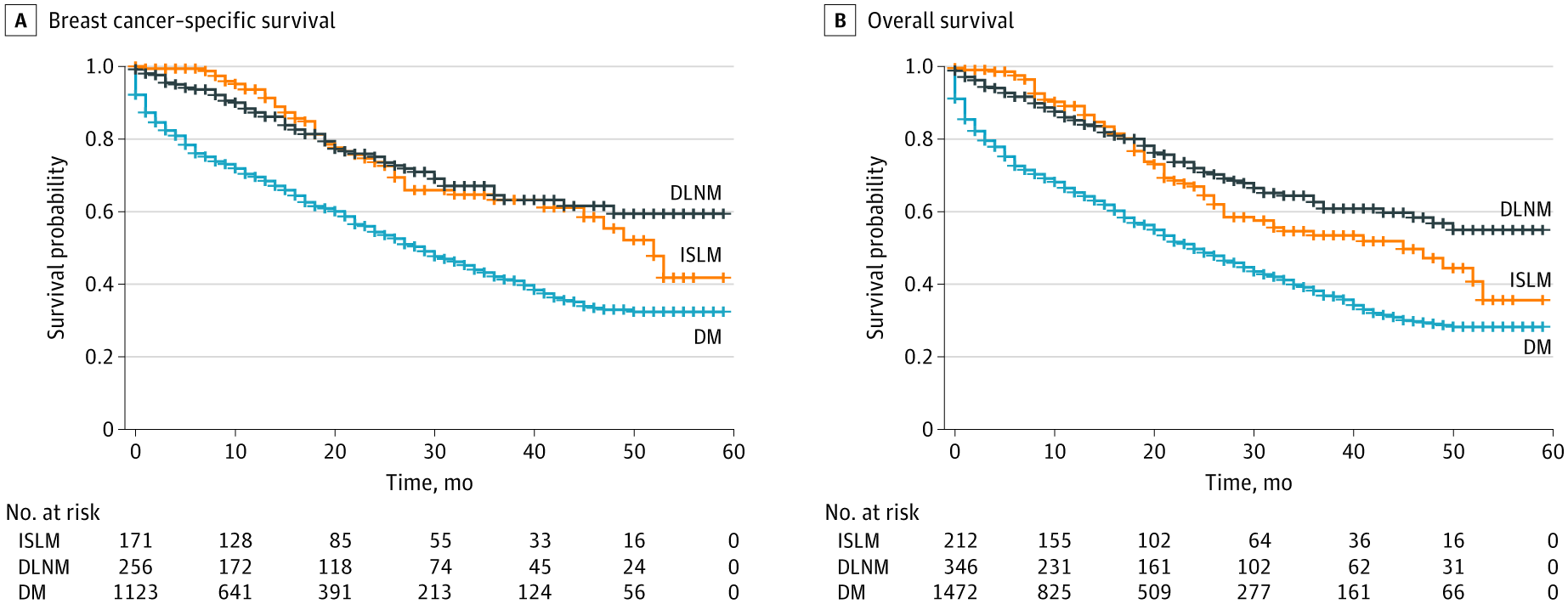
DLNM、ISLM和远处转移(DM)患者的Kaplan-Meier生存曲线
Ⅳ期乳腺癌仍然是一种几乎无法治愈的疾病,治疗的主要目标是延长生存期和减轻症状。全身治疗,包括化疗、内分泌治疗和抗ERBB2治疗,是Ⅳ期乳腺癌的主要治疗方法。Ⅰ~Ⅲ期乳腺癌是一种可治愈的疾病,局部治疗加或不加全身治疗是主要的治疗方法。在目前的队列研究中,研究者发现DLNM患者与任何亚型ISLM患者的生存率相当。DLNM患者目前可能是一种可治愈的疾病,该疾病可能被归类为N3疾病,而不是IV期疾病。
据研究者所知,这项队列研究首次从大样本中提供直接证据,表明患有DLNM的乳腺癌可能是一种可治愈的疾病,类似于N3c疾病,其预后明显优于其他类型的IV期疾病(DLNM除外)。局部治疗可显著提高DLNM患者的生存率。提示乳腺癌的DLNM可能是一种区域性疾病,而不是一种转移性疾病,有必要重新评估其在乳腺癌淋巴结转移中的作用。
参考文献:Pan H, Wang H, Qian M, et al. Comparison of Survival Outcomes Among Patients With Breast Cancer With Distant vs Ipsilateral Supraclavicular Lymph Node Metastases. JAMA Netw Open. 2021;4(3):e211809. doi:10.1001/jamanetworkopen.2021.1809
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#区域性#
44
#淋巴结#
28
#淋巴结转移#
44
#局部#
34
#局部治疗#
46
非常棒!
62
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
54