European Radiology:深度学习在CT结肠造影中良恶性息肉鉴别的应用。
2022-06-03 shaosai MedSci原创
计算机断层扫描(CT)结肠造影是一种无创的结肠癌筛查方法。对于检测≥6毫米的结肠息肉,CT结肠造影的敏感性与OC相当。
 结肠癌是全世界范围内最常见的与癌症有关的死亡原因之一。然而,通过生长数年的癌前腺瘤性息肉的早期发现,可大大降低死亡率和发病率。
结肠癌是全世界范围内最常见的与癌症有关的死亡原因之一。然而,通过生长数年的癌前腺瘤性息肉的早期发现,可大大降低死亡率和发病率。
计算机断层扫描(CT)结肠造影是一种无创的结肠癌筛查方法。对于检测≥6毫米的结肠息肉,CT结肠造影的敏感性与OC相当。计算机辅助检测(CAD)算法作为第二阅读器使用时,可以显著减少CT结肠造影漏掉的息肉数量。
然而,传统的CT结肠造影并不能明确区分良性和早期恶性的结直肠息肉,而这对于个人风险分层和治疗管理是至关重要的。恶性腺瘤性息肉需要内镜切除,而良性增生性息肉的发现则可以避免不必要的干预。由于息肉大小是CT结肠造影时恶性肿瘤可能性的唯一指标,目前的指南建议切除CT结肠造影中检测到的≥6毫米的结直肠息肉。
首批研究表明,使用放射组学的基于机器学习的CT结肠造影可以无创地区分良性和恶性前的结直肠息肉。使用卷积神经网络(CNN)的基于深度学习的图像分类不需要事先对感兴趣的区域进行分割,并被证明是自动图像分析的有效方法,为肿瘤成像中的肿瘤检测和分类提供了强有力的工具。
近日,发表在European Radiology杂志的一项研究利用深度学习建立了一个使用CT结肠造影进行早期恶性(即腺瘤)和良性(即增生性息肉或普通粘膜)结直肠息肉鉴别的诊断模型,为临床提供了一个强有力的评估结肠息肉的影像学手段。
在本项对平均风险结直肠癌筛查样本的回顾性分析中,所有大小类别和形态的息肉都在仰卧和俯卧的CT结肠造影图像上进行手动分割,并根据组织病理学划分为早期恶性(腺瘤)或良性(增生性息肉或正常粘膜)。两个深度学习模型SEG和noSEG在三维CT结肠造影图像子卷上进行训练,以预测息肉等级,模型SEG还使用息肉分割掩码进行训练。诊断性能在一个独立的外部多中心测试样本中得到验证。用可视化技术Grad-CAM++分析了预测结果。
训练集包括63名患者(平均年龄:63±8岁,40名男性)的107个结直肠息肉,包括169个息肉分割。外部测试集包括59名患者的77个息肉,包括118个息肉分段。SEG模型的ROC-AUC为0.83,区分恶性和良性息肉的敏感性为80%,特异性为69%。noSEG模型的ROC-AUC为0.75,敏感性为80%,特异性为44%,90%的息肉组织的Grad-CAM++热图平均得分≥0.25。
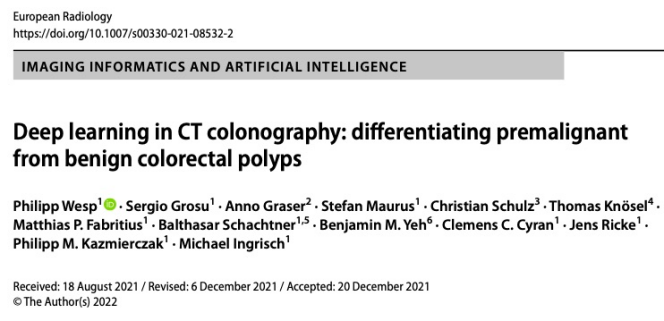
图 a-c 在轴向二维CT结肠造影图像(上排)和相应的虚拟透视三维重建图(下排)中显示的结直肠息肉(用箭头表示)。A,58岁女性直肠内7毫米的增生性息肉;b,74岁女性横结肠内8毫米的管状腺瘤;c,67岁男性直肠内9毫米的管状腺瘤
在本项概念验证研究中,基于深度学习的CT结肠造影分析可在一个与组织病理学相对应的外部验证队列中进行恶性和良性结直肠息肉的鉴别。即使模型只提供了CT图像且没有使用专家的息肉分割掩码,也可以进行区分。尽管研究结果需要在前瞻性研究中得到验证,但所提出的方法可促进高危息肉的早期无创识别。
原文出处:
Philipp Wesp,Sergio Grosu,Anno Graser,et al.Deep learning in CT colonography: differentiating premalignant from benign colorectal polyps.DOI:10.1007/s00330-021-08532-2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
42
#造影#
44
#学习##期刊论坛#
68
不错的文章
56