JAMA Oncol:卡巴他赛在转移性/局部晚期去分化脂肪肉瘤中的活性
2022-09-09 MedSci原创 MedSci原创
卡巴他赛在转移性或不可手术的局部晚期DDLPS患者中具有重要的活性
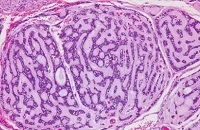
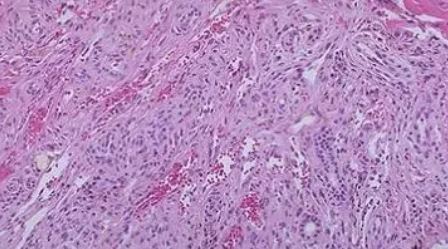
脂肪肉瘤 (LPS) 是成人软组织肉瘤最常见的组织学亚型。根据分子和临床特征,LPS可分为不同的亚型,包括高分化/去分化 (WD/DD) LPS、粘液样/圆形细胞LPS和多形性LPS。不可切除和/或转移性去分化脂肪肉瘤 (DDLPS) 患者的治疗选择有限。亟需新的治疗药物。
该研究目的是评估卡巴他赛在转移性或无法手术的局部晚期DDLPS患者中是否有足够的抗肿瘤活性。
这是一项国际性、多中心、开放标签、单臂的2期试验,招募了转移性或局部晚期的DDLPS患者,要求有在过去6个月内疾病进展的证据、既往化疗次数≤1次。予以卡巴他赛 25mg/m2 静滴,21天一次,直到不能耐受、进展或撤出试验。主要终点是12周时的无进展生存(PFS)率。
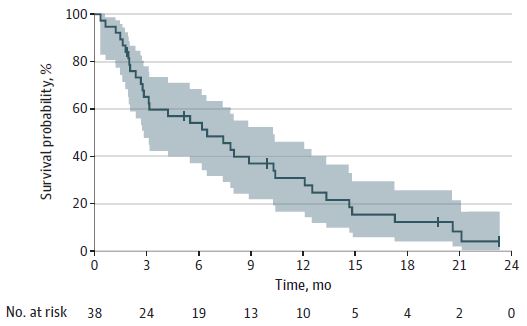
无进展生存率
筛查了40位患者,其中2位不符合纳入条件。中位治疗疗程是5个,范围是1-30个;26位(65%)患者至少接受了4个疗程的卡巴他赛治疗。12周时的无进展生存率是55%,达到了研究主要终点。中位随访了21.6个月,中位PFS是6个月,中位总生存期是21个月。缓解率是8%,包括1例临床缓解(CR)和2例部分缓解(PR)。23位(60.5%)患者的病情稳定(SD)。26位(68%)患者获得了疾病控制(部分缓解+SD)。
3-4级不良反应事件的发生情况
总之,该试验达到了其主要终点,12周内有21位患者的病情未发生进展。该研究结果提示卡巴他赛在转移性或不可手术的局部晚期DDLPS患者中具有重要的活性,值得开展3期试验进一步验证。
原始出处:
Sanfilippo R, Hayward RL, Musoro J, et al. Activity of Cabazitaxel in Metastatic or Inoperable Locally Advanced Dedifferentiated Liposarcoma: A Phase 2 Study of the EORTC Soft Tissue and Bone Sarcoma Group (STBSG). JAMA Oncol. Published online August 18, 2022. doi:10.1001/jamaoncol.2022.3218
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Oncol#
52
#局部晚期#
38
谢谢分享,学习了
27
#转移性#
45
#局部#
46
好文章,值得一读。
24