Radiology:在超低剂量胸部CT中,深度学习可实现肺结节的“既要、又要、还要”
2022-03-11 shaosai MedSci原创
据统计,肺癌是现阶段全球范围内癌症相关死亡的主要原因,占总数的18.4%。大量的CT筛查可以将肺癌的10年死亡率降低24%。尽管对肺癌筛查的需求迅速增加,但辐射暴露的累积负荷限制了其进一步的广泛应用。
 据统计,肺癌是现阶段全球范围内癌症相关死亡的主要原因,占总数的18.4%。大量的CT筛查可以将肺癌的10年死亡率降低24%。尽管对肺癌筛查的需求迅速增加,但辐射暴露的累积负荷限制了其进一步的广泛应用。在保证诊断准确性的前提下,尽可能地减少辐射剂量至关重要。然而,传统的图像重建方法并不能减少低剂量采集的图像噪声。现阶段,临床上引入了迭代重建,如ASIR-V和ADMIRE用来重建图像和减少噪声。在低剂量CT背景下,迭代重建可以显著减少图像噪声并提高图像质量。
据统计,肺癌是现阶段全球范围内癌症相关死亡的主要原因,占总数的18.4%。大量的CT筛查可以将肺癌的10年死亡率降低24%。尽管对肺癌筛查的需求迅速增加,但辐射暴露的累积负荷限制了其进一步的广泛应用。在保证诊断准确性的前提下,尽可能地减少辐射剂量至关重要。然而,传统的图像重建方法并不能减少低剂量采集的图像噪声。现阶段,临床上引入了迭代重建,如ASIR-V和ADMIRE用来重建图像和减少噪声。在低剂量CT背景下,迭代重建可以显著减少图像噪声并提高图像质量。
最近,临床上引入了基于卷积神经网络的深度学习图像重建(DLIR)技术以改善低剂量环境下的图像质量。近日,发表在Radiology杂志的一项研究比较了DLIR和ASIR-V在超低剂量(ULD)CT中的图像质量和肺部结节显示情况,在保证图像质量的同时进一步减少辐射剂量。
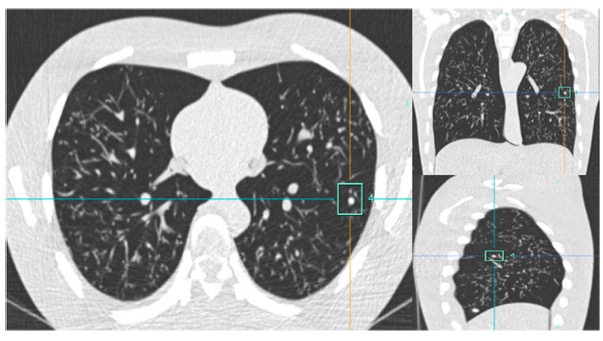
本研究对2020年4月至6月期间进行平扫ULD CT(在0.07或0.14 mSv下进行,类似于单张胸片)和对比增强胸部CT(CECT)扫描的患者被进行了评估。ULD CT图像用滤波背投(FBP)、ASIR-V和DLIR进行重建。对肺组织进行了三维分割以评估图像噪声。放射医师利用基于深度学习的结节评估系统检测和测量结节,并识别与恶性肿瘤相关的影像特征。用Bland-Altman分析和重复测量方差分析来评估ULD CT图像和CECT图像之间的差异。
共纳入203名参与者(平均年龄±标准差,61岁±12岁;129名男性),有1066个结节,其中100次扫描为0.07mSv,103次扫描为0.14mSv。CECT的平均肺组织噪声±标准差为46 HU±4,ULD CT扫描的FBP、ASIR-V水平40%、ASIR-V水平80%(ASIR-V-80%)、中等强度DLIR和高强度DLIR(DLIR-H)分别为59 HU±4、56 HU±4、53 HU±4、54 HU±4和51 HU±4(P < .001)。FBP重建、ASIR-V-80%和DLIR-H的结节检出率分别为62.5%(1066个结节中的666个)、73.3%(1066个结节中的781个)和75.8%(1066个结节中的808个)(P < .001)。Bland-Altman分析显示,在FBP重建、ASIR-V-80%和DLIR-H中,长径与CECT的百分比差异分别为9.3%(95%平均CI:8.0,10.6)、9.2%(95%平均CI:8.0,10.4)和6.2%(95%平均CI:5.0,7.4)(P < .001)。

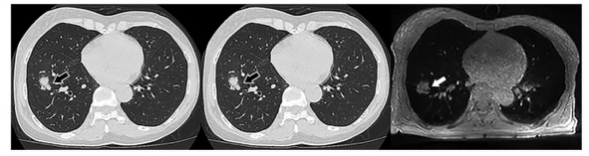
图 来自DLIR和ASIR-V的具有代表性胸部CT图像。72岁男性,体重指数为19.0kg/m2,5年前有右中叶肺癌手术的临床病史。这四张图像包括作为参考的CECT图像(使用ASIR-V 50%水平重建)和0.14mSv超低剂量CT下的滤波背投(FBP)、ASIR-V 80%水平(ASIR-V-80%)和高强度DLIR(DLIR-H)图像。红色勾勒的区域显示了肺实质的放大图像的细节。DLIR-H图像比ASIR-V-80%图像显示更清晰的肺实质和更多的细节,与CECT图像相似。
与ASIR-V相比,深度学习图像重建(DLIR)技术可通过减少图像噪声和提高肺部结节检测率来改善图像质量。DLIR还提高了结节测量的准确性,并显示了更详细的与恶性肿瘤相关的结节影像学特征。随着这种特定的DLIR算法的引入,在体重不足和体重正常的参与者中使用低至0.14 mSv的等效胸部CT采集来检测和描述肺部结节是可行的,这对于促进大规模肺癌筛查的临床实施至关重要。
原文出处:
Beibei Jiang,Nianyun Li,Xiaomeng Shi,et al.Deep Learning Reconstruction Shows Better Lung Nodule Detection for Ultra-Low-Dose Chest CT.DOI:10.1148/radiol.210551
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#胸部CT#
51
#低剂量#
48
分辨率,辨识度越来越强了
67
好东西,谢谢分享!
52
学习了
54