blood:免疫再生障碍性贫血的 HLA 关联、HLA 表达的体细胞丧失和临床结果。
2021-12-18 MedSci原创 MedSci原创
免疫性再生障碍性贫血(AA)是由一种破坏造血干细胞的T细胞引起的,骨髓衰竭通过造血细胞移植或免疫抑制治疗(IST)成功治疗。与单独使用IST相比,EPAG(EPAG)联合IST产生更高的血液学反应和生

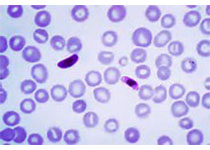
免疫性再生障碍性贫血(AA)是由一种破坏造血干细胞的T细胞引起的,骨髓衰竭通过造血细胞移植或免疫抑制治疗(IST)成功治疗。与单独使用IST相比,EPAG(EPAG)联合IST产生更高的血液学反应和生存率,但复发和克隆进化等长期结果在临床上仍存在问题,生物学上尚不清楚。AA 的特点是骨髓细胞上 HLA I 类等位基因表达的体细胞丧失,这与 T 细胞介导的造血干细胞和祖细胞破坏的逃逸机制一致,但HLA 异常的临床意义尚未得到很好的表征。
图1:研究患者和临床参数。根据数据的可用性,检测亚组中临床参数与HLA基因型和HLA损失的相关性。

图2:HLAI类等位基因缺失。
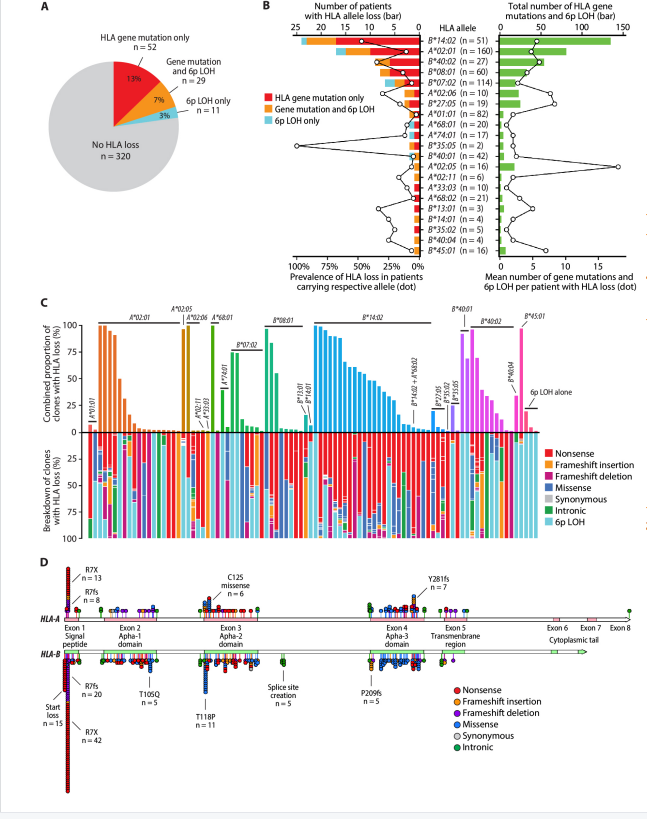
一研究团队检查了 HLA I 类等位基因的体细胞丢失,并将 HLA 丢失和突变相关的 HLA 基因型与 544 名 AA 患者的免疫抑制治疗后的临床表现和结果相关联。在接受测试的 412 名患者中,有 92 名 (22%) 检测到 HLA I 类等位基因丢失,其中有 393 个体细胞 HLA 基因突变和 40 个杂合性丢失实例。
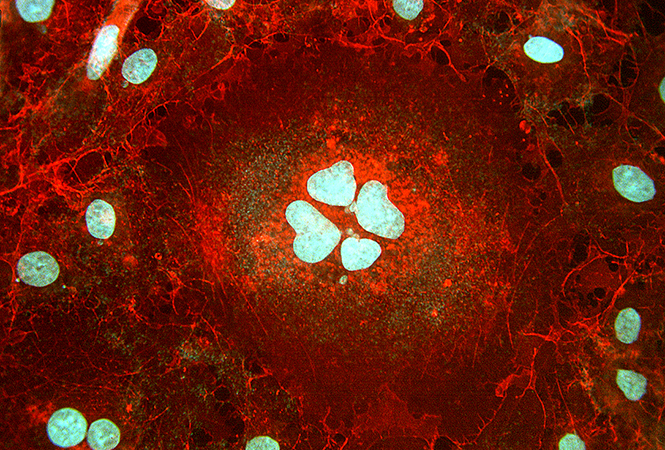
图3:高危克隆进化。
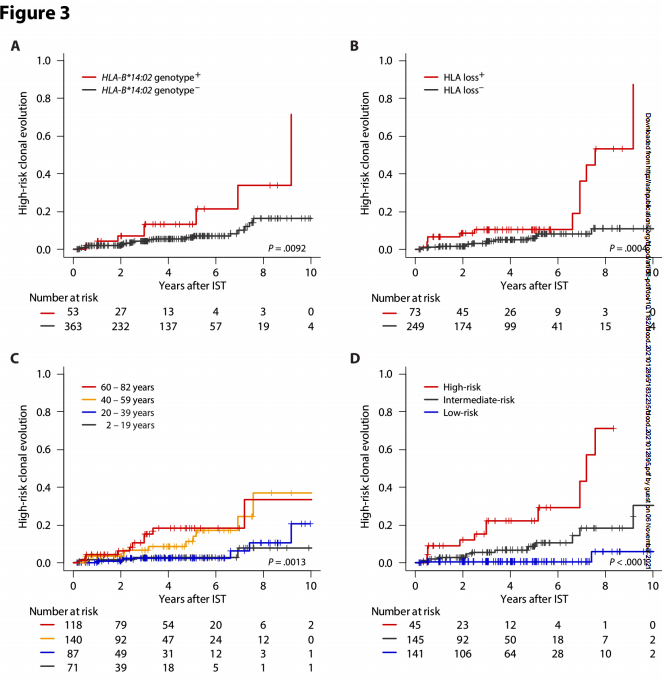
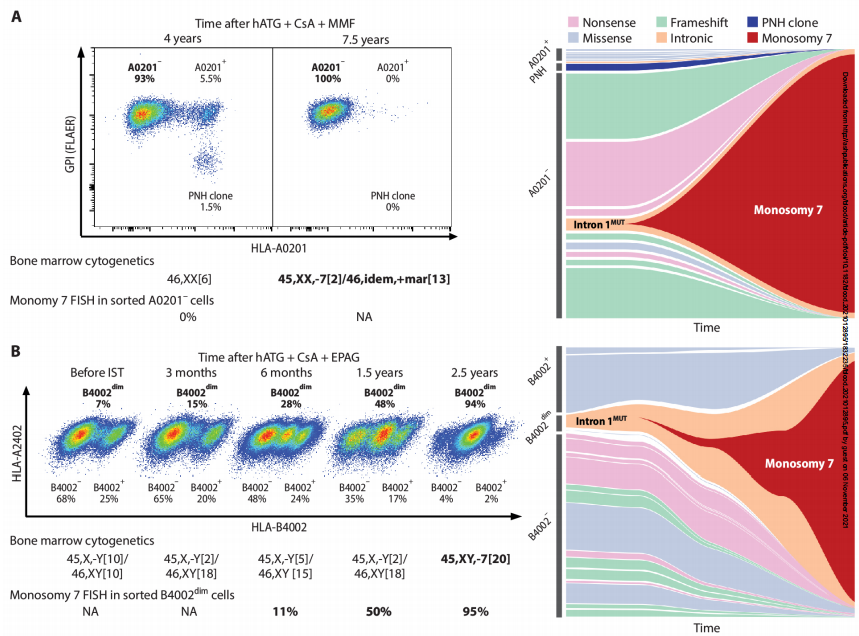
图4:缺乏克隆的HLAI类等位基因7的克隆进化。
最常受影响的是HLA-B*14:02,其次是HLA-A*02:01、HLA-B*40:02,HLA-B*08:01和HLA-B*07:02。HLA-B*14:02、HLA-B*40:02和HLA-B*07:02在 AA 中的比例也过高。高风险克隆进化与 HLA 缺失、HLA-B*14:02基因型和年龄较大相关,从而产生了有效的预测模型。
在两名患者中,研究者追踪了单体 7 克隆的进化,这些克隆来自在HLA-A*02:01和HLA-B*40:02 中携带体细胞突变的预先存在的克隆。HLA-B*40:02 的丢失与更高的血细胞计数相关。HLA-B*07:02和HLA-B*40:01基因型及其丢失与 AA 的晚发相关。
总的来说,这项研究表明存在与HLA基因型和免疫AA缺失相关的不同致病途径。临床中最重要的是高危恶性克隆进化与i类介导免疫之间的关系,如最常失活的HLA-b*14:02基因型和一般的HLA缺失,这为这一严重并发症提供了一个简单的预测工具。
原始出处:
Zaimoku Y, Patel BA, Adams SD, Shalhoub RN, Groarke EM, Lee AAC, Kajigaya S, Feng X, Rios OJ, Eager H, Alemu L, Quinones Raffo D, Wu CO, Flegel WA, Young NS. HLA associations, somatic loss of HLA expression, and clinical outcomes in immune aplastic anemia. Blood. 2021 Nov 1:blood.2021012895. doi: 10.1182/blood.2021012895. Epub ahead of print. PMID: 34724566.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#临床结果#
44
学习了
63
学习了
64
学到了
60
厉害#梅斯医学科研互助群#
63
#体细胞#
35
#HLA#
35