Neurology:机械取栓 vs 桥接治疗:前循环大血管闭塞卒中患者更倾向于使用BT,功能独立性、再灌注成功率、死亡率指标更优
2022-03-11 Naomi MedSci原创
汇总所有前循环LVO卒中患者研究数据,功能独立性、成功再灌注和死亡率的几率更倾向于使用BT而不是MT。当分析局限于随机对照试验时,两种治疗方法的功能和安全性结果相似(无异质性),但再通率有利于BT组。
几个国家和国际专业组织建议对症状出现1-3个小时内的缺血性卒中患者使用静脉溶栓(IVT)。以往的随机对照试验(RCT)已证实机械取栓术(MT)治疗大血管闭塞(LVO)所致的前循环卒中患者具有良好的疗效和安全性。对于符合这两种治疗条件的患者,目前的指南建议IVT后再进行MT(又名桥接疗法[BT])。IVT在实现LVO后再通方面的疗效有限,有报道认为IVT可能延迟MT的启动,导致血栓碎裂和远端迁移,并增加症状性出血(SICH)的风险。因此,几个小组已经调查了BT与MT单独治疗LVO患者的有效性和安全性。先前比较BT和MT的观察性研究的Meta分析表明BT是有利的。然而,这些研究的解释被包括后循环卒中、选择偏差和研究设计中的变化所混淆。
最近发表了三项新的 RCT 比较 LVO 患者的接受 BT 与 MT 治疗的结果。这三项研究的荟萃分析显示两种治疗的功能独立性和死亡率相当,但与单独接受 MT 的患者相比,血栓切除术(BT)前的 IVT 导致成功再通的可能性更高。这些研究是在亚洲人群中进行的,并且限制了将患者招募到具有 MT 能力的中心,这些因素限制了结果的普遍性。此外,一些方法学因素混淆了结果的解释,包括未能满足预先指定的一项研究中的非劣效性边缘,以及另一项研究的提前终止。将 MT 与 BT 进行比较的第四项 RCT 的初步结果已在 2021 年国际卒中会议上公布,最终结果最近发表。这项研究也未能证明两种治疗方法之间的非劣效性或优越性。包括这四项 RCT 的荟萃分析发现,BT 增加了成功再灌注的几率。最近,在 2021 年世界卒中大会上公布了另外两项研究 BT 与 MT 对比的RCT 结果。对于同时符合 MT 和 IVT 条件的患者的最佳治疗,临床平衡仍然存在。近日,有研究人员通过汇总迄今为止在前循环 LVO 卒中患者中进行的所有观察性和随机研究的数据,比较 BT 与 MT 的疗效和安全性。
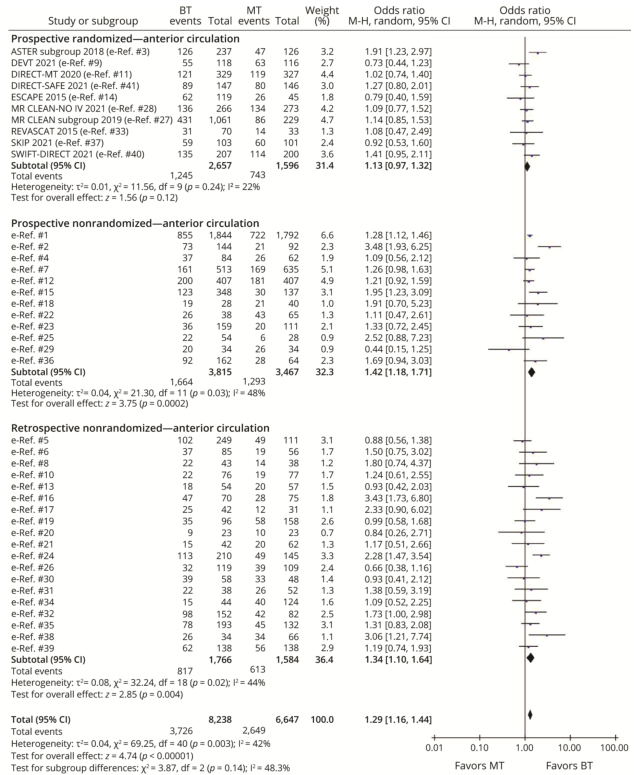
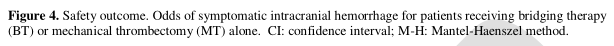
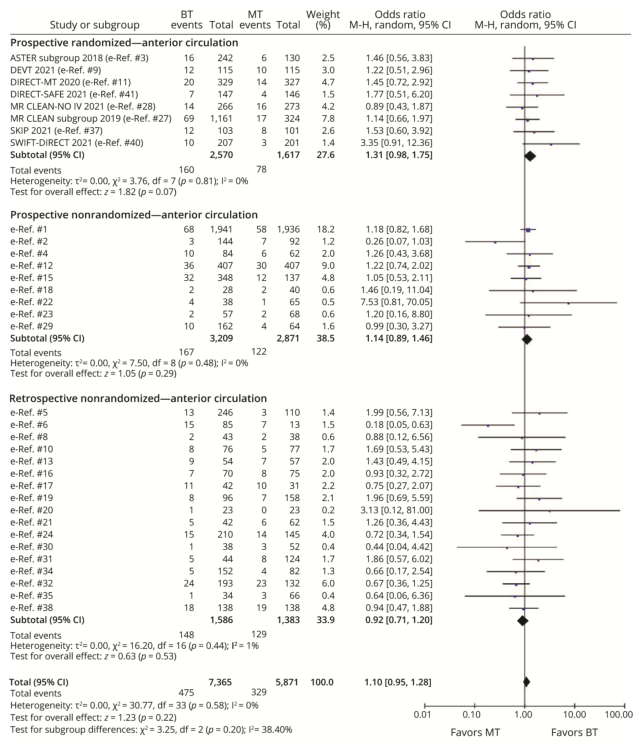
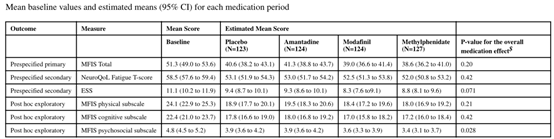
对2021年10月29日至2021年10月29日的生物医学文献数据库进行系统搜索,以确定前瞻性和回顾性研究,比较MT和BT的功能独立性(改良Rankin评分0~2分)和90天死亡率、症状性出血(SICH)和成功率。效果大小用优势比(OR)表示,用随机效应Meta分析进行分析。用I2和Cochrane‘s Q统计量评价异质性。
- 总共纳入了41项研究,涉及14885名患者。BT组平均年龄±标准差为69±11岁,MT组为70±11岁。所有研究均采用阿替普酶作为溶栓剂。
- 与MT相比,BT组功能独立的优势比MT高29%(OR=1.29,95%CI 1.16~1.44,I2=42%),再灌注成功的优势比MT高25%(OR=1.25,95%CI=1.08~1.44,I2=42%),死亡率比MT低31%(OR=0.69,95%CI.60~0.80,I2=47%)。两组间患病率相似(OR=1.10,95%CI=0.95~1.28,I2=0%)。
- 其中6项研究是随机临床试验(RCT),对直接到MT中心就诊的患者进行意向治疗分析。当仅对这6项随机对照试验(n=2333)进行分析时,两组间的功能独立性(OR=1.08,95%CI=0.91~1.27,I2=0%)、SICH(OR=1.37,95%CI=0.95~1.97,I2=0%)或死亡率(OR=0.93,95%CI=0.74~1.16,I2=0%)均无差异。然而,BT组再灌注成功率更优(OR=1.35,95%CI=1.06~1.73,I2=0%)。
整个数据集的功能独立性、成功再灌注和死亡率的几率更倾向于使用BT而不是MT(中等异质性和低质量的证据)。当分析局限于随机对照试验时,两种治疗方法的功能和安全性结果相似(无异质性),但再通率有利于BT组(无异质性)。由于这些发现在不具备MT能力的中心或使用其他溶栓剂的患者中可能有所不同,因此需要进一步的随机对照试验。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言




















#独立性#
32
#Neurol#
40
#血管闭塞#
43
#卒中患者#
38
#大血管#
34
#取栓#
40
#机械取栓#
45