Cancers:帕妥珠单抗和曲妥珠单抗联合局部放疗治疗HER2阳性乳腺癌患者的疗效和安全性
2021-09-27 yd2015 MedSci原创
该研究表明,局部乳腺放疗(RT)与帕妥珠单抗/曲妥珠单抗双HER2阻断联合使用具有良好的耐受性,提示HER2阳性乳腺癌患者可以安全加入RT。
HER2受体(人表皮生长因子受体2)过表达存在于15 - 30%的乳腺癌中。曲妥珠单抗是首个针对HER2受体的人源化单克隆抗体,其在 HER2阳性乳腺癌中的疗效已被证实。帕妥珠单抗也是一种人源化抗HER2单克隆抗体。在转移性HER2阳性乳腺癌患者中,帕妥珠单抗和曲妥珠单抗双重HER2阻断联合局部乳腺放疗是重要的一种治疗策略。但是其疗效和安全性还不是很明确。近期,Cancers杂志发表了相关回顾性研究结果。
研究最终纳入55例患者,患者中位年龄为53岁(范围:28 - 81岁)。绝大多数患者(94.5%)的肿瘤组织学为浸润性导管癌。患者多为晚期疾病,58.2%为T3 -4期,58.2%为N+期,58.2%为高级别肿瘤,58.2%为3级。4例(7.3%)患者在放疗前有心血管病史。
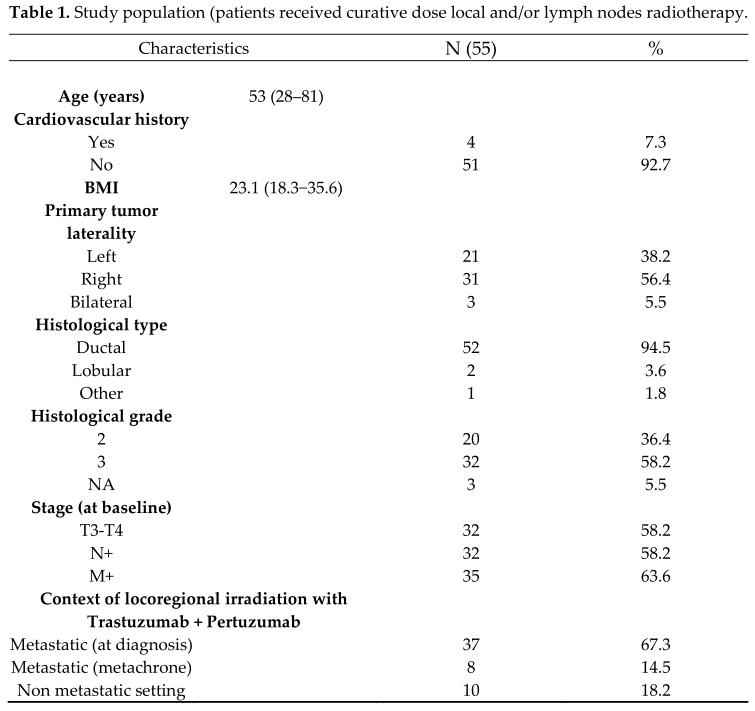
临床特征
帕妥珠单抗/曲妥珠单抗双HER2阻断治疗时,所有患者均曾接受过化疗,其中多西他赛(69.1%)、紫杉醇(9.1%)和表柔比星(14.5%)。共10例(18.2%)患者未行手术,23例(41.8%)患者行肿瘤切除术,19例(34.5%)患者行乳房切除术。放疗中位剂量为50Gy EQD2(范围:40 Gy -74 Gy)。
皮肤毒性:早期中毒包括3例(5.4%)3级和14例(25.5%)2级自发性放射性皮炎。其余患者发生0级和1级毒性反应(69.1%)。迟发性毒性为1例(1.8%)2级毛细血管扩张。胃肠毒性:在放疗期间观察到1例(1.8%)早期1级食管炎。心脏毒性:在联合治疗期间未观察到心脏事件。在治疗开始和结束之间,LVEF下降了2.43%(17% +14%),具有统计学意义。没有患者同时经历大于10%的LVEF下降,同时LVEF<55%。左侧放疗后LVEF下降为65%(55% 73%),右侧放疗后LVEF下降为65% (48% 77%)(p = 0.39)。没有肺部或甲状腺相关毒性报道。
放疗后的中位随访时间为4.1年。4年总生存率(OS)为81.7%(69.5% -96.2%)。

OS
4年无进展生存率(PFS)为65.7%(51.7%-83.6%)。

PFS
4年局部无复发生存率(LRRFS)为97.1%(91.5%-100%)。中位OS、PFS和LRRFS均未达到。
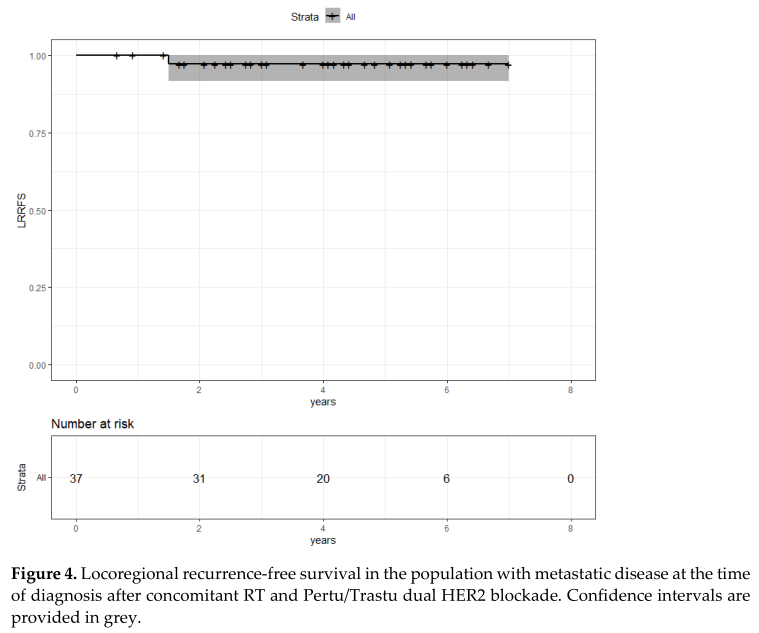
局部无复发生存率(LRRFS)
综上,该研究表明,局部乳腺放疗(RT)与帕妥珠单抗/曲妥珠单抗双HER2阻断联合使用具有良好的耐受性,提示HER2阳性乳腺癌患者可以安全加入RT。
原始出处:
Aboudaram, A.; Loap, P.;Loirat, D.; Dhia, S.B.; Cao, K.; etal. Pertuzumab and Trastuzumab Combination with Concomitant Locoregional Radiotherapy for the Treatment of Breast Cancers with HER2 Receptor Overexpression. Cancers 2021, 13,4790. https://doi.org/10.3390/cancers 13194790
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ERS#
30
#曲妥珠#
40
#疗效和安全性#
29
#HER2阳性#
41
#局部#
27
#乳腺癌患者#
34