Front Oncol:吡咯替尼+长春瑞滨VS拉帕替尼+卡培他滨用于转移性HER-2阳性经治乳腺癌患者的疗效对比:多中心回顾性研究
2021-09-18 yd2015 MedSci原创
该回顾性研究表明,吡咯替尼+长春瑞滨(NP)较拉帕替尼+卡培他滨(LX)可改善经治转移性HER-2阳性乳腺癌患者的PFS。
吡咯替尼(Pyrotinib)是一种新型泛ErbB受体酪氨酸激酶抑制剂,在前期的临床研究中对于转移性HER2乳腺癌患者表现出了较好的疗效和安全性。在III期临床研究PHOEBE中证实,吡咯替尼+卡培他滨较拉帕替尼+卡培他滨(LX)改善晚期HER2+乳腺癌患者的无进展生存期(PFS)(p<0.001)。我们知道,口服长春瑞滨常与抗HER2治疗联合使用。然而,真实世界研究中还没有报道吡咯替尼+长春瑞滨(NP)对比LX的疗效和安全性。因此,复旦大学附属肿瘤医院王碧芸教授开展了回顾性研究,评估吡咯替尼+长春瑞滨(NP) VS拉帕替尼+卡培他滨(LX)用于转移性HER-2阳性经治乳腺癌患者的疗效。相关结果发表在Frontiers in Oncology杂志上,研究表明吡咯替尼联合长春瑞滨具有更好的PFS。
该研究为回顾性研究(NCT04850625),多中心筛选了自2015年6月至2021年1月期间所有接受了NP或LX治疗的转移性乳腺癌患者,入组标准包括需经病理证实为HER2阳性转移性乳腺癌,既往接受过曲妥珠单抗和紫杉烷类治疗。
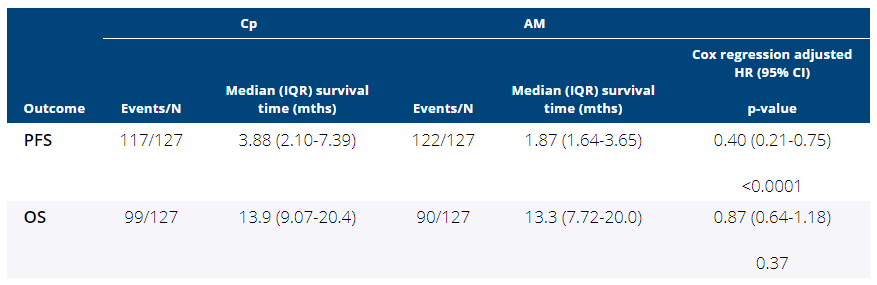
研究纳入224例患者,其中132例(58.9%)患者接受LX, 92例(41.1%)患者接受NP。中位随访时间20个月。NP组的中位无进展生存期(mPFS)明显长于LX组(8.3个月vs 5.0个月,HR = 0.47 95% CI 0.34-0.65, p <0.001)。数据分析时中位OS尚未达到。

PFS
根据曲妥珠单抗耐药状态进行分析发现,曲妥珠单抗耐药时,NP 和LX组的mPFS 分别为9.6个月和5.0个月(HR=0.30, 95% CI 0.16–0.57, p < 0.001);而曲妥珠单抗非耐药时,NP 和LX组的mPFS 分别为6.3个月和5.0个月(HR=0.58, 95% CI 0.39–0.86, p = 0.004)。

曲妥珠单抗不同耐药状态的PFS
亚组分析中,NP相对于LX的PFS优势在大多数亚组中都可以观察到,包括不同年龄组、DFI长度、内脏转移状态和ER/PR状态。
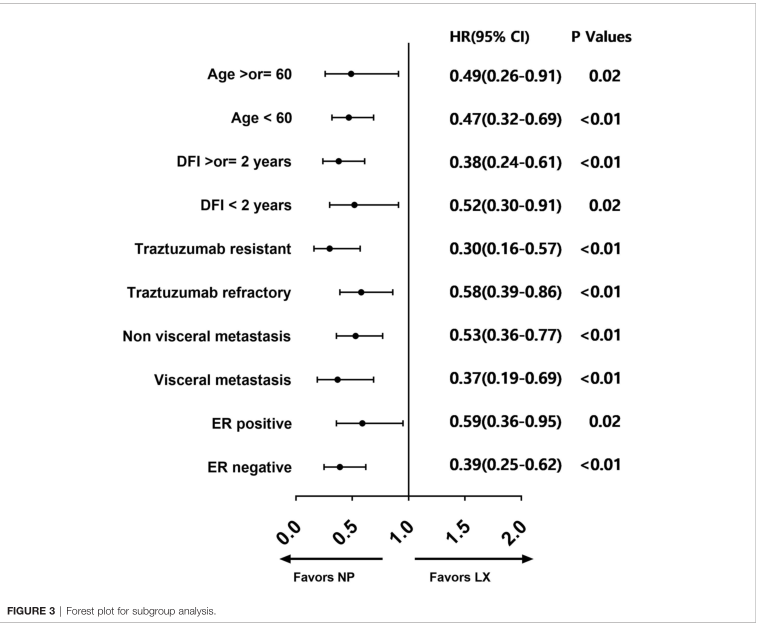
亚组分析
NP组腹泻发生率(23.9%)高于LX组(8.3%),而LX组手足综合征发生率(4.5 vs 0%)和丙氨酸氨基转移酶升高(2.3 vs 0%)高于NP组。两组有相似的血液毒性和疲劳。NP组9例(9.8%),LX组10例(7.8%)因毒性退出治疗,其他患者继续治疗。所有不良事件经对症治疗后均得到逆转,无患者因不良反应死亡。总的来说,两种治疗方案的安全性都是可以接受的。
综上,该回顾性研究表明,吡咯替尼+长春瑞滨(NP)较拉帕替尼+卡培他滨(LX)可改善经治转移性HER-2阳性乳腺癌患者的PFS。
原始出处:
Xie Y, Li Y, Ting L, et al. Pyrotinib Plus Vinorelbine Versus Lapatinib Plus Capecitabine in Patients With Previously Treated HER2-Positive Metastatic Breast Cancer: A Multicenter, Retrospective Study. Front Oncol. 2021 Aug 5;11:699333. doi: 10.3389/fonc.2021.699333. PMID: 34422652; PMCID: PMC8374067.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Oncol#
45
#多中心#
40
#卡培他滨#
57
#转移性#
33
#拉帕替尼#
55
#HER-2#
45
#乳腺癌患者#
29
#回顾性研究#
41
谢谢梅斯分享这么多精彩信息
71
认真学习了
70