气管插管是一种高风险操作,紧急插管通常在危重病患者中进行,但对插管导致的不良事件的了解却相对较少。与手术插管患者相比,危重症患者因潜在的休克、呼吸衰竭和代谢性酸中毒风险导致插管相关并发症风险增加。小规模研究中,在接受气管插管的危重病人中,28%可能会出现呼吸抑制并发症,如严重低氧血症或血流动力学不稳定,2.7%出现心脏骤停。

近日研究人员评估了危重病人插管期间不良事件的发生率和性质。
INTUBE研究旨在了解气道管理对危重病人的影响和最佳做法,研究时间为2018年10月1日到2019年7月31日,样本来自五大洲29个国家的197个ICU中心。研究的主要结果是主要不良插管事件的发生率,定义为插管开始后30分钟内发生以下事件:心血管指标不稳定(包括:心脏收缩压<65 mm Hg,持续30分钟以上的收缩压<90 mm Hg,使用血管升压类药物或剂量>15ml/kg),严重低氧血症(外周血氧饱和度<80%)或心脏骤停。次要结果为重症监护病房死亡率。
2964名患者参与研究,平均年龄63岁,62.6%为男性。52.3%的患者因出现呼吸衰竭而插管, 30.5%因神经损伤插管,9.4%因心血管指标不稳定而插管。研究中,45.2%的患者至少经历过一次主要的不良插管事件,主要原因是心血管指标不稳定,其中42.6%的紧急插管患者出现心血管指标不稳定。其次是严重低氧血症(9.3%)和心脏骤停(3.1%)。ICU总死亡率为32.8%。
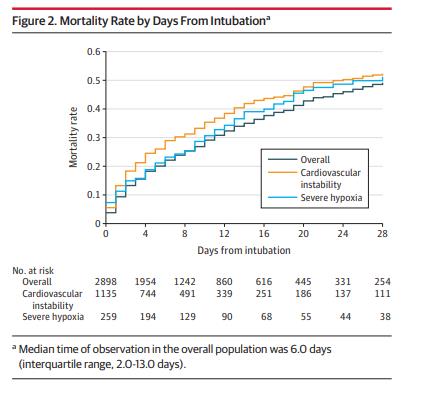
研究发现,危重病人插管后不良事件率近50%,最常见的是心血管指标不稳定。
原始出处
Vincenzo Russotto et al. Intubation Practices and Adverse Peri-intubation Events in Critically Ill Patients From 29 Countries.JAMA.March 24,2021.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#发生率#
23
#JAMA#点击进入话题查看更多相关文章 或评论时插入话题加入讨论
95
学习了
0
学习了
76
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
47