Heart:瓣膜性风湿心脏病孕妇不良心脏事件的预测
2020-07-22 MedSci原创 MedSci原创
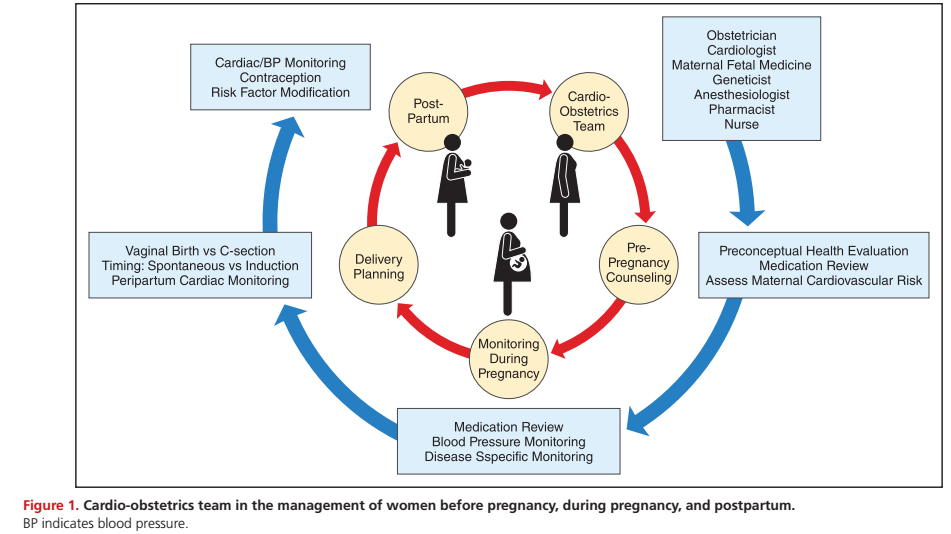
心力衰竭仍然是妊娠或产褥期最常见的不良心脏事件。将病变特定的特征和临床信息结合到一个简单有效的预测评分中,可用于常规临床实践。
近日,心脏病领域权威杂志Heart上发表了一篇研究文章,这项研究旨在评估风湿性心脏瓣膜病(RHD)孕妇不良心脏事件的发生率,并对其进行临床风险评分。
这是一项观察性研究,受试者为印度南部一家三级医院就诊的RHD孕妇。研究人员收集了受试者出院前的产科史、病史、母亲并发症和围产期结局的数据。分析中包括了681名妇女中的800次妊娠。该研究的主要结局为复合不良心脏事件,定义为发生一种或多种并发症,例如死亡、心脏骤停、心力衰竭、血栓栓塞和新发心律失常引起的脑血管意外。
在681名RHD妇女中,有180名(26.3%)被诊断为妊娠。122例(14.9%)孕妇发生妊娠/产后复合不良心脏结局,其中12例死于该疾病。在多变量分析中,先前的不良心脏事件(OR=8.35,95%CI为3.54至19.71)、心脏药物(OR=0.53,95%CI为0.32至0.86)、二尖瓣狭窄(轻度OR=2.48,95%CI为1.08至5.69;中度OR=2.23,95%CI为1.19至4.18;严重OR=7.72,95%CI为4.05至12.89)、瓣膜置换术(OR=2.53,95%CI为1.28至5.02)和肺动脉高压(OR=6.90,95%CI为3.81至12.46)可以预测复合不良心脏事件,并具有良好的辨别力(曲线下面积=0.803),并具有可以接受的校准性能。建议将这些因素结合在一起的预测评分可用于临床。
由此可见,心力衰竭仍然是妊娠或产褥期最常见的不良心脏事件。将病变特定的特征和临床信息结合到一个简单有效的预测评分中,可用于常规临床实践。
原始出处:
Jyoti Baghel.et al.Prediction of adverse cardiac events in pregnant women with valvular rheumatic heart disease.heart.2020.https://heart.bmj.com/content/early/2020/07/21/heartjnl-2020-316648
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










学习
40
#瓣膜性#
35
#心脏事件#
30
#ART#
29
#HEART#
24
#瓣膜#
33
学习
79
不错
74