ASCO GU 2021: ctDNA检测能有效判断Olaparib对去势抵抗性前列腺癌效果(PROfound研究)
2021-02-17 MedSci原创 MedSci原创
在转移性去势抵抗性前列腺癌(mCRPC)中,同源重组修复(HRR)通路基因突变(如BRCA1和BRCA2)有更强的疾病侵袭性和更高的死亡率。这类基因突变对聚二磷酸腺苷核糖聚合酶(PARP)抑制剂更敏感
在转移性去势抵抗性前列腺癌(mCRPC)中,同源重组修复(HRR)通路基因突变(如BRCA1和BRCA2)有更强的疾病侵袭性和更高的死亡率。这类基因突变对聚二磷酸腺苷核糖聚合酶(PARP)抑制剂更敏感,PARP抑制剂奥拉帕利用于HRR基因突变的mCRPC患者的疗效已在PROfound研究中证实。
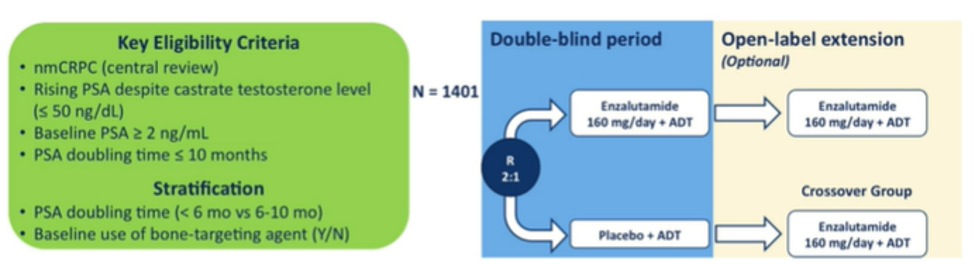
早期数据支持使用TOPARP-A试验中的PARP抑制剂olaparib(奥拉帕利),发现经mCRPC大量治疗的男性的无进展生存率和总体生存率均有改善。在II期TOPARP-B试验中观察到了相似的结果,随后在III期PROfound试验中得到了证实,该试验证明了在接受醋酸阿比特龙酯或enzalutamide治疗后,具有同源重组修复缺陷型mCRPC的男性的无进展生存期和总体生存期得到改善。与新型口服雄激素轴靶向药物相比,接受奥拉帕尼治疗的非转移性去势抵抗性前列腺癌的转移时间或转移性去势抵抗性前列腺癌的转移时间。纳入该试验需要同源重组修复(HRR)基因改变的证据,通常是通过肿瘤组织测试确定的。但是,ctDNA检测也可能允许检测HRR状态。在2021年ASCO GU癌症研讨会的海报重点会议:前列腺癌会议的全体摘要中,Matsubara博士及其同事对ctDNA进行了回顾性评估,以鉴定PROfound试验中男性BRCA1,BRCA2和ATM的改变。
PROfound的方法先前已有报道和发表,但总而言之,患有转移性去势抵抗性前列腺癌的男性在非转移性去势抵抗性前列腺癌或非转移性去势抗性前列腺癌时,曾服用过醋酸阿比特龙或恩杂鲁胺已进展。募集了转移性去势敏感性前列腺癌。允许先前有紫杉烷暴露的患者。然后研究人员使用了基于FoundationOne CDx的研究测定方法,以鉴定参与同源重组修复的15个预先指定基因之一的改变(BRCA 1/2,ATM,BRIP1,BARD1,CDK12,CHEK 1/2,FANCL,PALB2 ,PPP2R2A,RAD51B,RAD51C,RAD51D,RAD54L)。
PROfound研究是一项Ⅲ期、随机对照研究,纳入携带1-15个HRR基因突变、既往经二代抗雄药物(恩扎卢胺、阿比特龙)治疗进展的mCRPC患者。根据生物标记物驱动的分层,分为两个队列。队列A患者至少携带BRCA1、BRCA2或ATM基因突变其中之一,队列B至少携带其他15个基因突变(BRIP1、BARD1、CDK12、CHEK1、CHEK2、FANCL、PALB2、PPP2R2A、RAD51B、RAD51C、RAD51D、RAD54L)其中之一。
两个队列患者按2:1随机分配至奥拉帕利组(300mg 2次/天)或对照组(恩扎卢胺组【160mg 1次/天】、阿比特龙【1000mg 1次/天】+泼尼松【5mg 2次/天】组),若对照组发生疾病进展,可交叉至奥拉帕利组。在每个生物标记层中,根据之前使用紫杉烷类药物和可测量的疾病负担(根据RESIST 1.1标准)对随机分组进行分层。
队列A的主要终点为影像学无进展生存期(rPFS),OS为次要终点,次要终点还包括随机分组至第二次进展或死亡的时间。OS最终分析截至日期为2020年3月20日。
此前结果呈现,最终分析时,队列A的245名患者中有148名(60%)患者死亡,符合预先设定的标准。奥拉帕利组的中位OS为19.1个月,对照组为14.7个月(HR,0.69;95% CI:0.50-0.97;P=0.02)。67%的对照组患者在进展后交叉至奥拉帕利组,校正后HR=0.42(95% CI:0.19-0.91)。
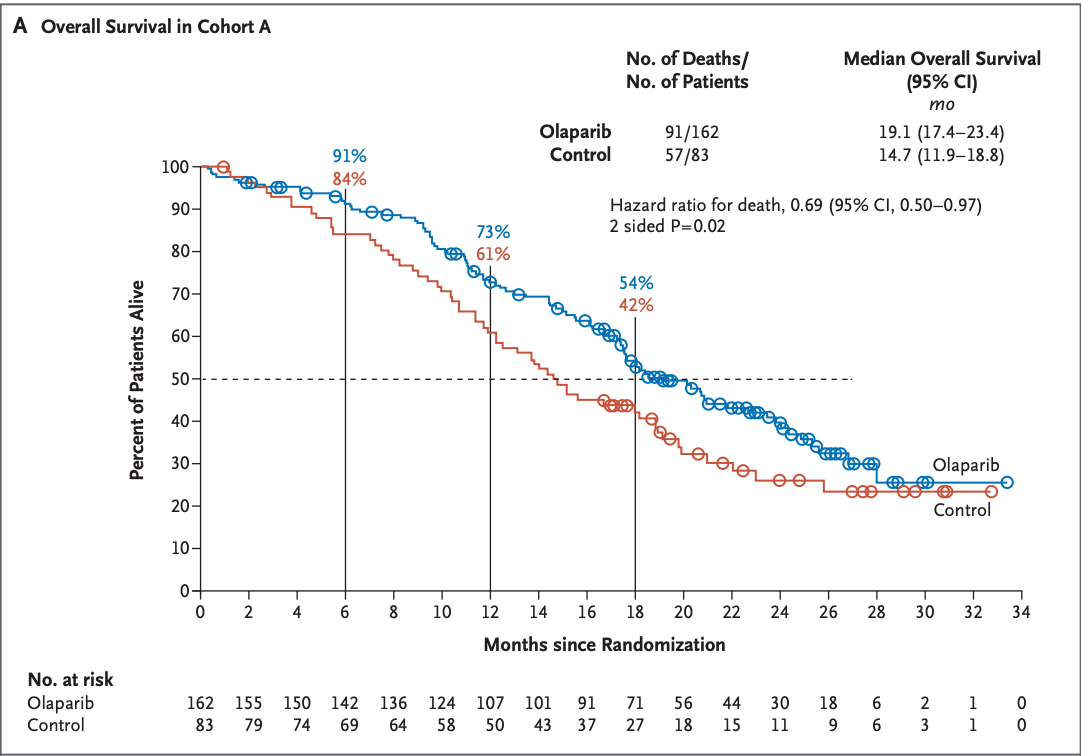
图1 队列A OS

图2 队列A校正交叉因素后OS
队列B的142名患者中有100名(70%)患者死亡。奥拉帕利组的中位OS为14.1个月,对照组为11.5个月(HR,0.96;95% CI:0.63-1.49)。校正交叉因素后,HR=0.83(95% CI:0.11-5.98)。基于临床前数据,无法验证PPP2R2A作为HRR基因的作用,在PPP2R2A基因突变的患者中,与对照组相比,奥拉帕利未观察到生存优势。在事后探索性分析中,排除队列B的这些患者后,HR=0.79(95% CI:0.51-1.25),奥拉帕利组和对照组的中位OS分别为14.2个月和10.8个月。
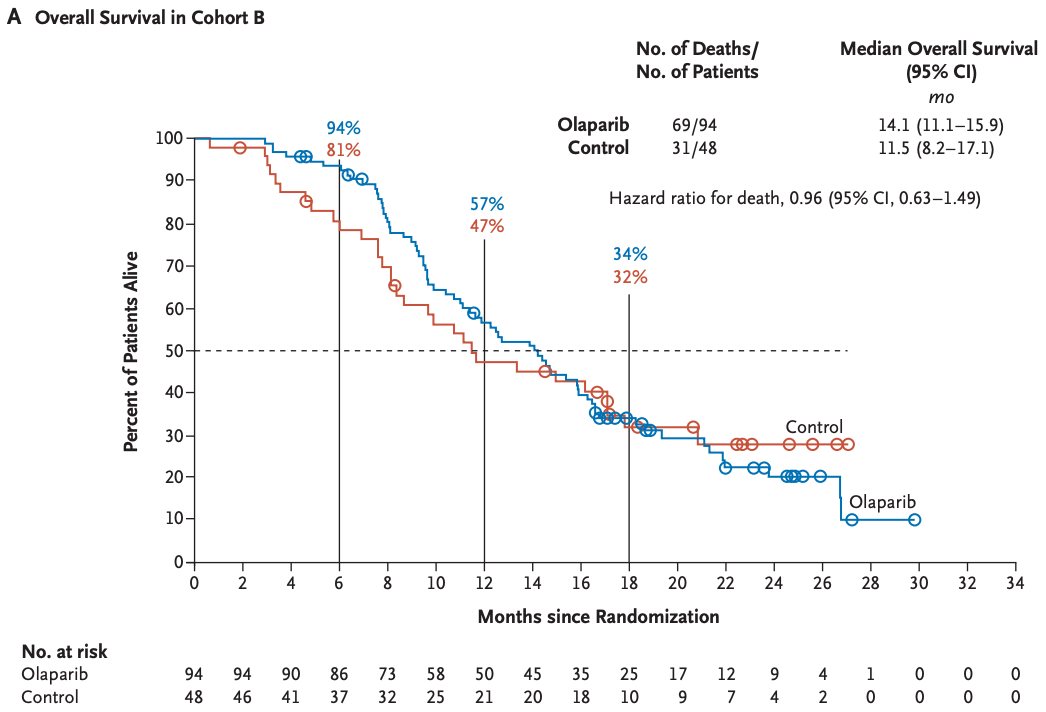
图3 队列B OS

图4 队列B校正交叉因素后OS
整体人群而言,387名患者中有248名(64%)患者死亡,奥拉帕利组和对照组的中位OS分别为17.3个月和14.0个月(HR,0.79;95% CI:0.61-1.03)。校正交叉因素后,HR=0.55(95% CI:0.29-1.06)。敏感性分析中,排除PPP2R2A基因突变患者,HR=0.76(95% CI:0.58-1.00),奥拉帕利组和对照组的中位OS分别为17.4个月和13.6个月。
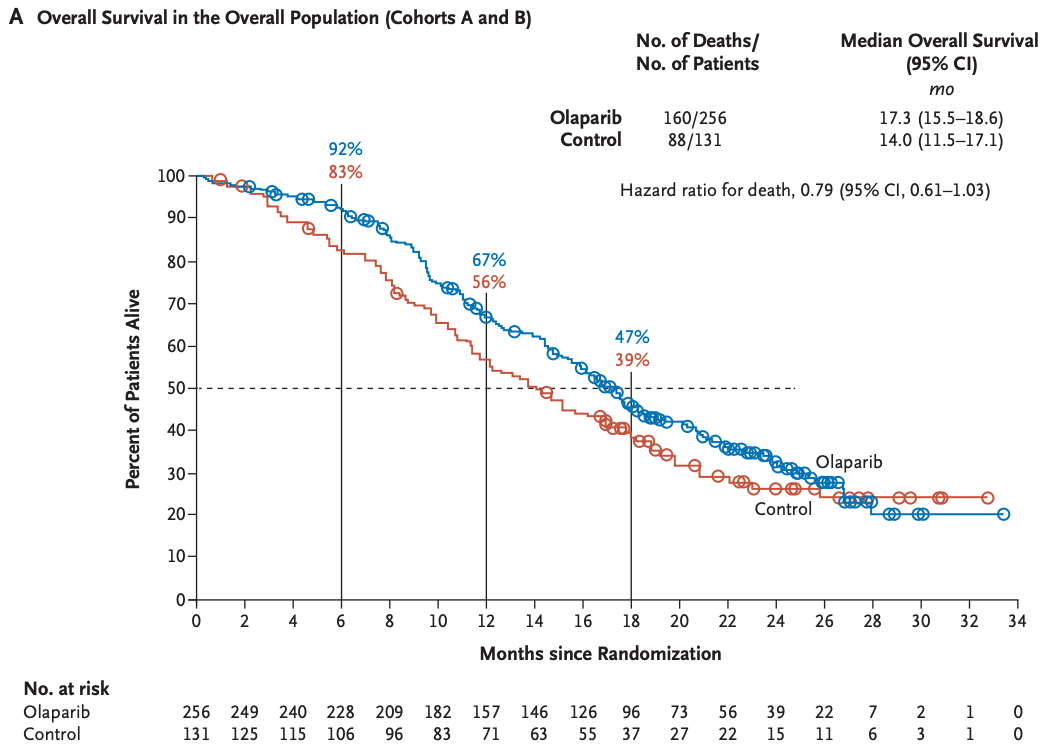
图5 整体人群OS(队列A+队列B)

图6 整体人群校正交叉因素后OS
本次在会议上报告的是ctDNA检测的价值。
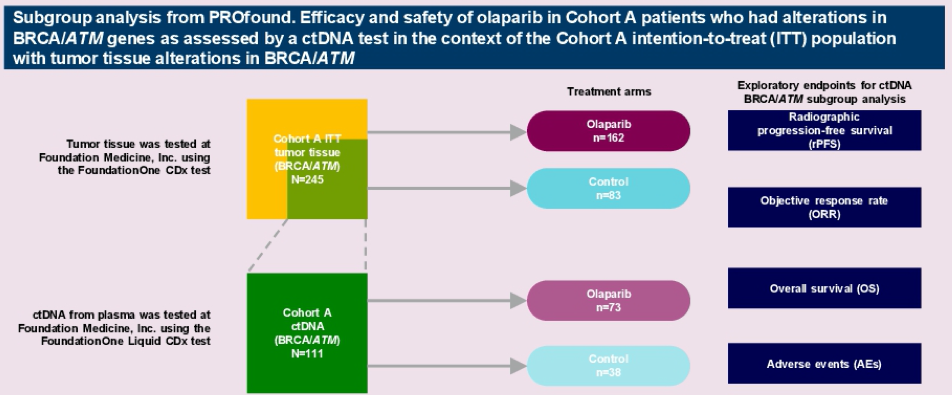
在这项分析中,作者检查了同意并提供了队列A血浆样本的患者(通过组织检测BRCA / ATM改变呈阳性)。 ctDNA样品在FMI上测序,使用在PROfound中筛选期间收集的血浆样品,通过FoundationOne Liquid CDx分析对BRCA1,BRCA2(BRCA)和ATM进行改变。 与该研究的主要终点一致,通过分层对数秩检验对由ctDNA改变阳性的患者进行了无盲独立中央评价(BICR)评估的无影像学无进展生存期(rPFS)。 还评估了其他次要功效终点(客观缓解率[ORR],总体生存率[OS])。
在队列A的245名患者中,有181名(73.9%)同意并提供了用于ctDNA检测的血浆样品,其中139/181名(76.8%)报告了ctDNA结果(突变阳性或突变阴性),其中42名患者 样品由于DNA产量不足或测试技术失败而无法通过测试。
在111/139(79.9%)的患者中鉴定出BRCA / ATM改变,其余28位患者在ctDNA测试中未报告BRCA / ATM突变,这归因于缺乏从肿瘤中脱落的ctDNA或低于检测灵敏度的ctDNA水平。 在BRCA / ATM ctDNA发生改变的人群与整个队列A中,BRCA1,BRCA2和ATM突变的人口统计学,基线特征和比例相似。
与研究者选择的抗雄激素转换相比,在具有ctDNA BRCA / ATM改变的患者中,接受Olaparib的患者的rPFS明显更长。
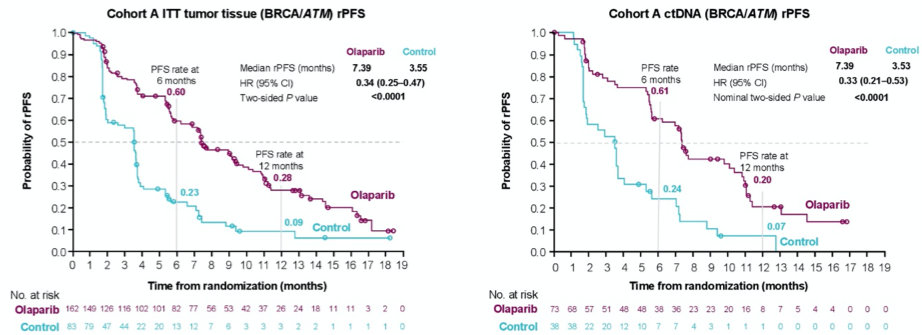
作者得出结论,在mCRPC患者中进行ctDNA检测既可行,而且在很大程度上与基于组织的HRR突变状态评估相一致。 此外,在基于ctDNA鉴定为具有BRCA / ATM改变的患者与整个队列A中的患者之间,对Olaparib的反应相似。
原始出处:
Hussain M, Mateo J, Fizazi K, Saad F, Shore N, Sandhu S, Chi KN, Sartor O, Agarwal N, Olmos D, Thiery-Vuillemin A, Twardowski P, Roubaud G, Özgüroğlu M, Kang J, Burgents J, Gresty C, Corcoran C, Adelman CA, de Bono J; PROfound Trial Investigators.Survival with Olaparib in Metastatic Castration-Resistant Prostate Cancer.N Engl J Med. 2020 Dec 10;383(24):2345-2357
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#ASC#
45
#抗性#
47
#olaparib#
43
#DNA检测#
55
#LAP#
53
#APA#
37
#去势抵抗性前列腺癌#
25
#PRO#
32
前列腺癌相关研究,学习了,谢谢梅斯
46
疗效只是效果的众多方面之一,还要看对患者的获益,包括生活质量等因素共同决定效果的
46