Clinica Chimica Acta:导致LPAC综合征的纯合子ABCB4突变演变为胆管癌
2019-10-17 gladiator MedSci原创
ABCB4突变和低胆道磷脂浓度与症状性和复发性胆石症相关是低磷脂相关胆石症(LPAC)的特征。
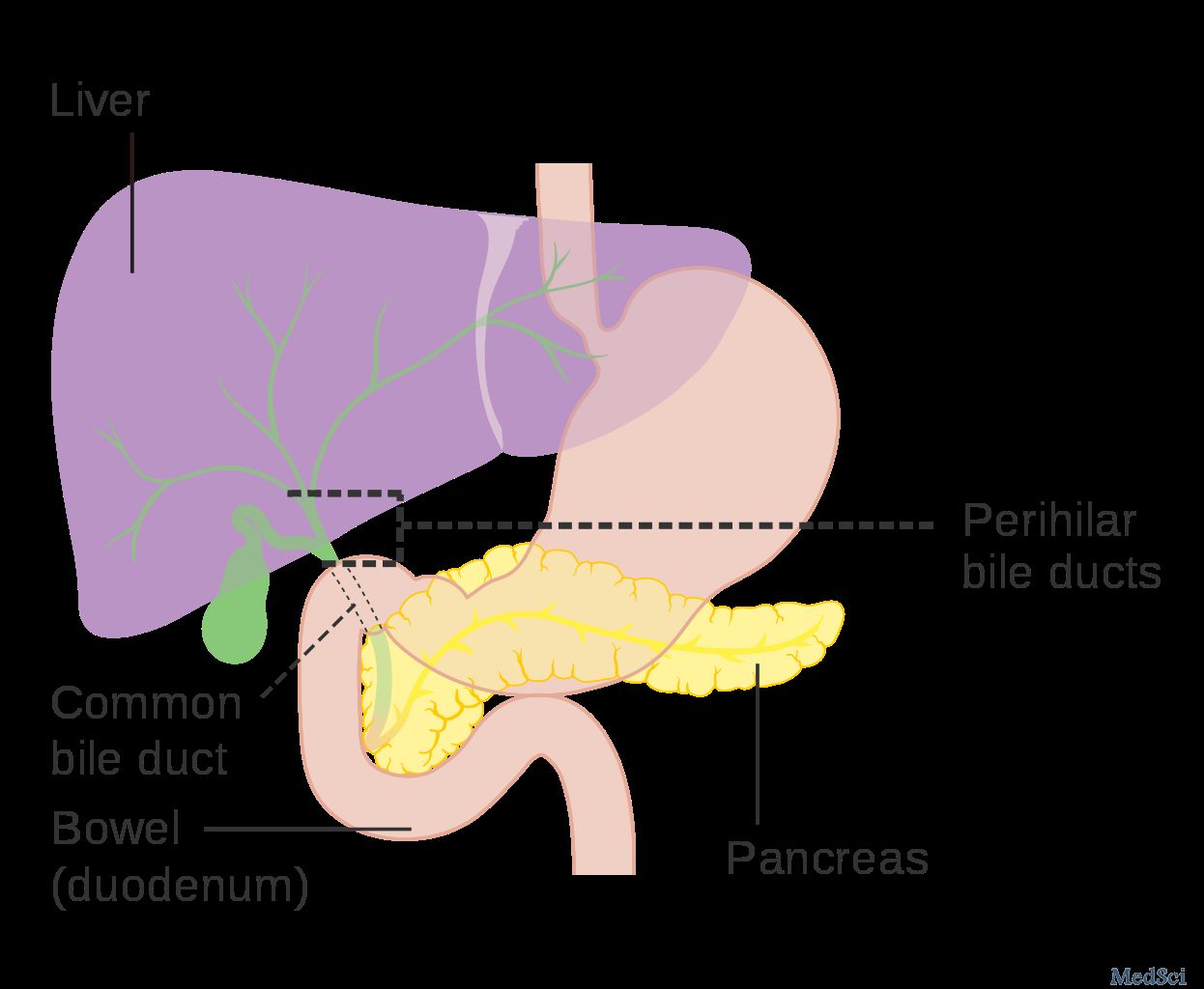
ABCB4突变和低胆道磷脂浓度与症状性和复发性胆石症相关是低磷脂相关胆石症(LPAC)的特征。在本研究中,我们报告了一例63岁女性患者,她在30岁时开始出现胆道疼痛,胆囊切除术后复发,并伴有超声显示的“彗星尾影”,从而实现了对LPAC的诊断。这种疾病发展成胆管癌。为了了解这种表型的分子基础,我们进行了ABCB4基因测序,然后进行了电脑预测分析和Q-RT-PCR检测。结果显示了纯合错义序列的变异(c.140G > A,
p.Arg47Gln),根据MutPred预测为致病。因此,这导致了肝脏ABCB4 mRNA水平的降低和突变蛋白的结构改变。最后,我们在这里报告了突尼斯LPAC综合征中第一个关于纯合子状态的ABCB4错义突变(p.Arg47Gln)。对其功能结果进行了说明。此外,本病例提示LPAC综合征的延迟诊断和UDCA治疗的缺乏可能导致胆管癌等并发症的发生。
原始出处:
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#演变#
33
#ABC#
27
#CTA#
32
#综合征#
36
#LPA#
33
#胆管#
30